ผลลัพธ์ของไนโทรฟูแรนโทอินในการรักษาโรคติดเชื้อทางเดินปัสสาวะชนิดไม่ซับซ้อน
คำสำคัญ:
ไนโทรฟูแรนโทอิน, โรคติดเชื้อทางเดินปัสสาวะชนิดไม่ซับซ้อนบทคัดย่อ
ความเป็นมา: เชื้อก่อโรคติดเชื้อทางเดินปัสสาวะชนิดไม่ซับซ้อนที่พบบ่อยคือ Escherichia coli, Klebsiella pneumoniae ซึ่งพบว่าเชื้อดื้อต่อยารักษาหลักคือ โคไทรม็อกซาโซลและนอร์ฟล็อกซาซิน มากกว่าร้อยละ 20 จึงจำเป็นต้องหายาปฏิชีวนะที่เหมาะสมมาทดแทน
วัตถุประสงค์: เพื่อเปรียบเทียบผลลัพธ์ของไนโทรฟูแรนโทอินในการรักษาโรคติดเชื้อทางเดินปัสสาวะชนิดไม่ซับซ้อน กับยาปฏิชีวนะกลุ่ม beta-lactams, fluoroquinolones, sulfonamides
วิธีการวิจัย: เป็นการศึกษาแบบพรรณนาย้อนหลังเปรียบเทียบผลลัพธ์ทางคลินิก ผลลัพธ์ทางจุลชีววิทยา และการเกิดเป็นซ้ำ ระหว่างกลุ่มผู้ป่วยที่ได้รับการรักษาด้วยไนโทรฟูแรนโทอิน จำนวน 127 รายกับกลุ่มที่ได้รับยาปฏิชีวนะกลุ่ม beta-lactams, fluoroquinolones, sulfonamides จำนวน 325 ราย ในระหว่าง เมษายน ถึง กันยายน พ.ศ. 2563
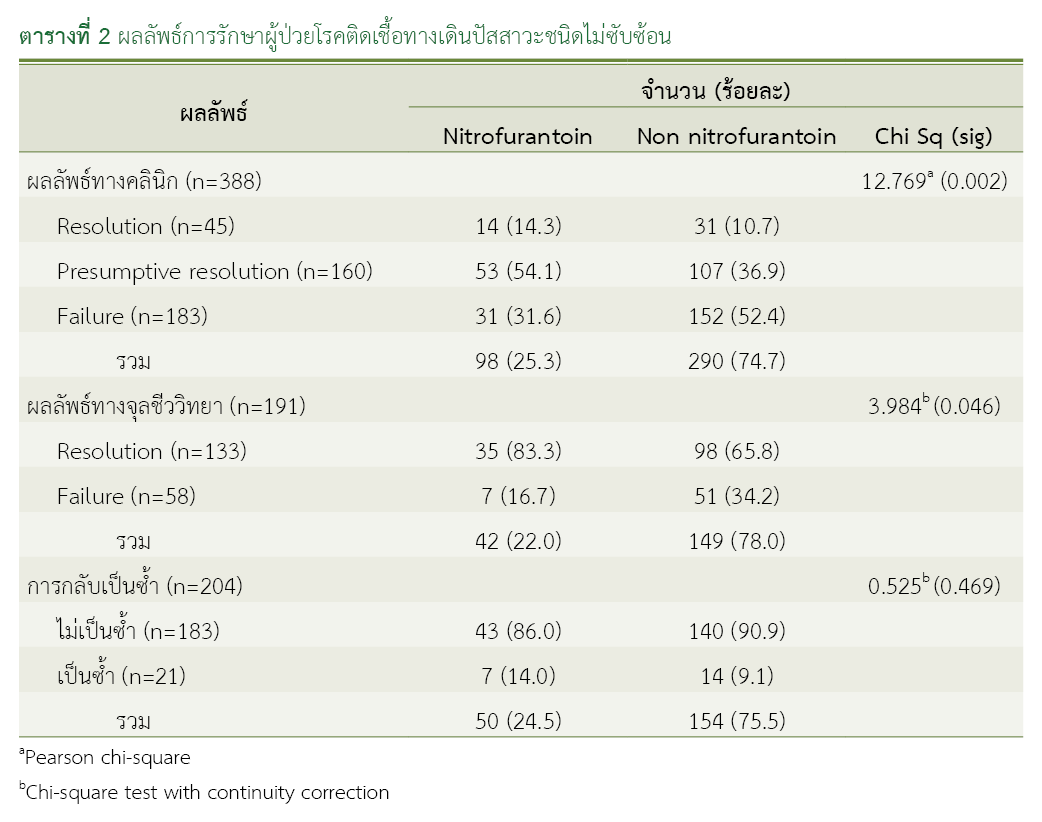
ผลการวิจัย: จากกลุ่มตัวอย่างทั้งหมด 452 ราย พบว่ากลุ่มตัวอย่างที่ได้รับไนโทรฟูแรนโทอิน (127 ราย) ให้ผลการรักษาโรคติดเชื้อทางเดินปัสสาวะชนิดไม่ซับซ้อนหายร้อยละ 14.3 มากกว่าการรักษาด้วยยาปฏิชีวนะกลุ่ม beta-lactams, fluoroquinolones, sulfonamides (325 ราย) ที่ให้ผลหายร้อยละ 10.7 แตกต่างอย่างมีนัยสำคัญทางสถิติ (p-value = 0.002) และตรวจไม่พบเชื้อในปัสสาวะสูงกว่าอย่างมีนัยสำคัญทางสถิติ (p-value = 0.046) ร้อยละ 83.3 และร้อยละ 65.8 พบว่าการกลับเป็นซ้ำทั้ง 2 กลุ่มไม่แตกต่างกัน คือ ร้อยละ 14.0 และ ร้อยละ 9.1 (p-value = 0.469)
สรุปผล: ไนโทรฟูแรนโทอินมีประสิทธิภาพดีกว่ายาปฏิชีวนะอื่น ๆ เหมาะสมเป็นยาทางเลือกแรกในการรักษาโรคติดเชื้อทางเดินปัสสาวะชนิดไม่ซับซ้อน
เอกสารอ้างอิง
Bader MS, Loeb M, Leto D, Brooks AA. Treatment of urinary tract infections in the era of antimicrobial resistance and new antimicrobial agents. Postgrad Med. 2020;132(3):234-50. doi: 10.1080/00325481.2019.1680052.
Ten Doesschate T, van Haren E, Wijma RA, Koch BCP, Bonten MJM, van Werkhoven CH. The effectiveness of nitrofurantoin, fosfomycin and trimethoprim for the treatment of cystitis in relation to renal function. Clin Microbiol Infect. 2020;26(10):1355-60. doi: 10.1016/j.cmi.2020.03.001.
Al-Zahrani J, Al Dossari K, Gabr AH, Ahmed AF, Al Shahrani SA, Al-Ghamdi S. Antimicrobial resistance patterns of uropathogens isolated from adult women with acute uncomplicated cystitis. BMC Microbiol. 2019;19(1):237. doi: 10.1186/s12866-019-1612-6.
Wawrysiuk S, Naber K, Rechberger T, Miotla P. Prevention and treatment of uncomplicated lower urinary tract infections in the era of increasing antimicrobial resistance-non-antibiotic approaches: a systemic review. Arch Gynecol Obstet. 2019;300(4):821-8. doi: 10.1007/s00404-019-05256-z.
Sangsuwan T, Jamulitrat S, Phengmak M. Nitrofurantoin and fosfomycin susceptibility among outpatient uropathogens in a tertiary care center in southern Thailand. J Health Sci Med Res. 2018;36(2):135–45; doi: 10.31584/jhsmr.2018.36.2.7.
Pedela RL, Shihadeh KC, Knepper BC, Haas MK, Burman WJ, Jenkins TC. Preferential use of nitrofurantoin over fluoroquinolones for acute uncomplicated cystitis and outpatient Escherichia coli resistance in an integrated healthcare system. Infect Control Hosp Epidemiol. 2017;38(4):461-8. doi: 10.1017/ice.2016.315.
Percival KM, Valenti KM, Schmittling SE, Strader BD, Lopez RR, Bergman SJ. Impact of an antimicrobial stewardship intervention on urinary tract infection treatment in the ED. Am J Emerg Med. 2015;33(9):1129-33. doi: 10.1016/j.ajem.2015.04.067.
Howard B, Furman B. Nitrofurantoin. In: Reference module in biomedical sciences. n.p.: Elsevier; 2018. p.1-5. doi: 10.1016/B978-0-12-801238-3.98024-3.
Mahdizade Ari M, Dashtbin S, Ghasemi F, Shahroodian S, Kiani P, Bafandeh E, et al. Nitrofurantoin: properties and potential in treatment of urinary tract infection: a narrative review. Front Cell Infect Microbiol. 2023;13:1148603. doi: 10.3389/fcimb.2023.1148603.
Wijma RA, Fransen F, Muller AE, Mouton JW. Optimizing dosing of nitrofurantoin from a PK/PD point of view: what do we need to know? Drug Resist Updat. 2019;43:1-9. doi: 10.1016/j.drup.2019.03.001.
Lodhia S, Sharaf A, Foley C. Management of recurrent urinary tract infections in adults. Surgery (Oxford). 2020;38(4):197–203. doi: 10.1016/j.mpsur.2020.01.012.
Huttner A, Kowalczyk A, Turjeman A, Babich T, Brossier C, Eliakim-Raz N, et al. Effect of 5-day nitrofurantoin vs single-dose fosfomycin on clinical resolution of uncomplicated lower urinary tract infection in women: a randomized clinical trial. JAMA. 2018;319(17):1781-9. doi: 10.1001/jama.2018.3627.
Gupta K, Hooton TM, Naber KG, Wullt B, Colgan R, Miller LG, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011;52(5):e103-20. doi: 10.1093/cid/ciq257.
McKinnell JA, Stollenwerk NS, Jung CW, Miller LG. Nitrofurantoin compares favorably to recommended agents as empirical treatment of uncomplicated urinary tract infections in a decision and cost analysis. Mayo Clin Proc. 2011;86(6):480-8. doi: 10.4065/mcp.2010.0800.
ดาวน์โหลด
เผยแพร่แล้ว
วิธีการอ้างอิง
ฉบับ
บท
การอนุญาต
ลิขสิทธิ์ (c) 2025 กองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
ข้อความภายในบทความที่ตีพิมพ์ในวารสารเภสัชกรรมคลินิกทั้งหมด รวมถึงรูปภาพประกอบ ตาราง เป็นลิขสิทธิ์ของกองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข การนำเนื้อหา ข้อความหรือข้อคิดเห็น รูปภาพ ตาราง ของบทความไปจัดพิมพ์เผยแพร่ในรูปแบบต่าง ๆ เพื่อใช้ประโยชน์ในเชิงพาณิชย์ ต้องได้รับอนุญาตจากกองบรรณาธิการวารสารเภสัชกรรมคลินิกอย่างเป็นลายลักษณ์อักษร
กองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข อนุญาตให้สามารถนำไฟล์บทความไปใช้ประโยชน์และเผยแพร่ต่อได้ โดยอยู่ภายใต้เงื่อนไขสัญญาอนุญาตครีเอทีฟคอมมอน (Creative Commons License: CC) โดย ต้องแสดงที่มาจากวารสาร – ไม่ใช้เพื่อการค้า – ห้ามแก้ไขดัดแปลง, Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0)
ข้อความที่ปรากฏในบทความในวารสารเป็นความคิดเห็นส่วนตัวของผู้เขียนแต่ละท่านไม่เกี่ยวข้องกับกองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข และบุคลากรในกองฯ หรือ ชมรมฯ แต่อย่างใด ความรับผิดชอบองค์ประกอบทั้งหมดของบทความแต่ละเรื่องเป็นของผู้เขียนแต่ละท่าน หากมีความผิดพลาดใด ๆ ผู้เขียนแต่ละท่านจะรับผิดชอบบทความของตนเอง ตลอดจนความรับผิดชอบด้านเนื้อหาและการตรวจร่างบทความเป็นของผู้เขียน ไม่เกี่ยวข้องกับกองบรรณาธิการ



