Factors Associated with Efficacy of Calcium Polystyrene Sulfonate among Patients with Mild Hyperkalemia
Keywords:
hyperkalemia, calcium polystyrene sulfonate, factors, spironolactone, glomerular filtration rateAbstract
Background: Patients with mild hyperkalemia should be promptly treated with calcium polystyrene sulfonate (CPS) to reduce their serum potassium levels to normal rapidly and to prevent increasing to the level that affects life. However, in some cases, serum potassium levels may not decrease to the normal range despite the treatment.
Objective: To investigated factors associated with efficacy of CPS among patients with mild hyperkalemia.
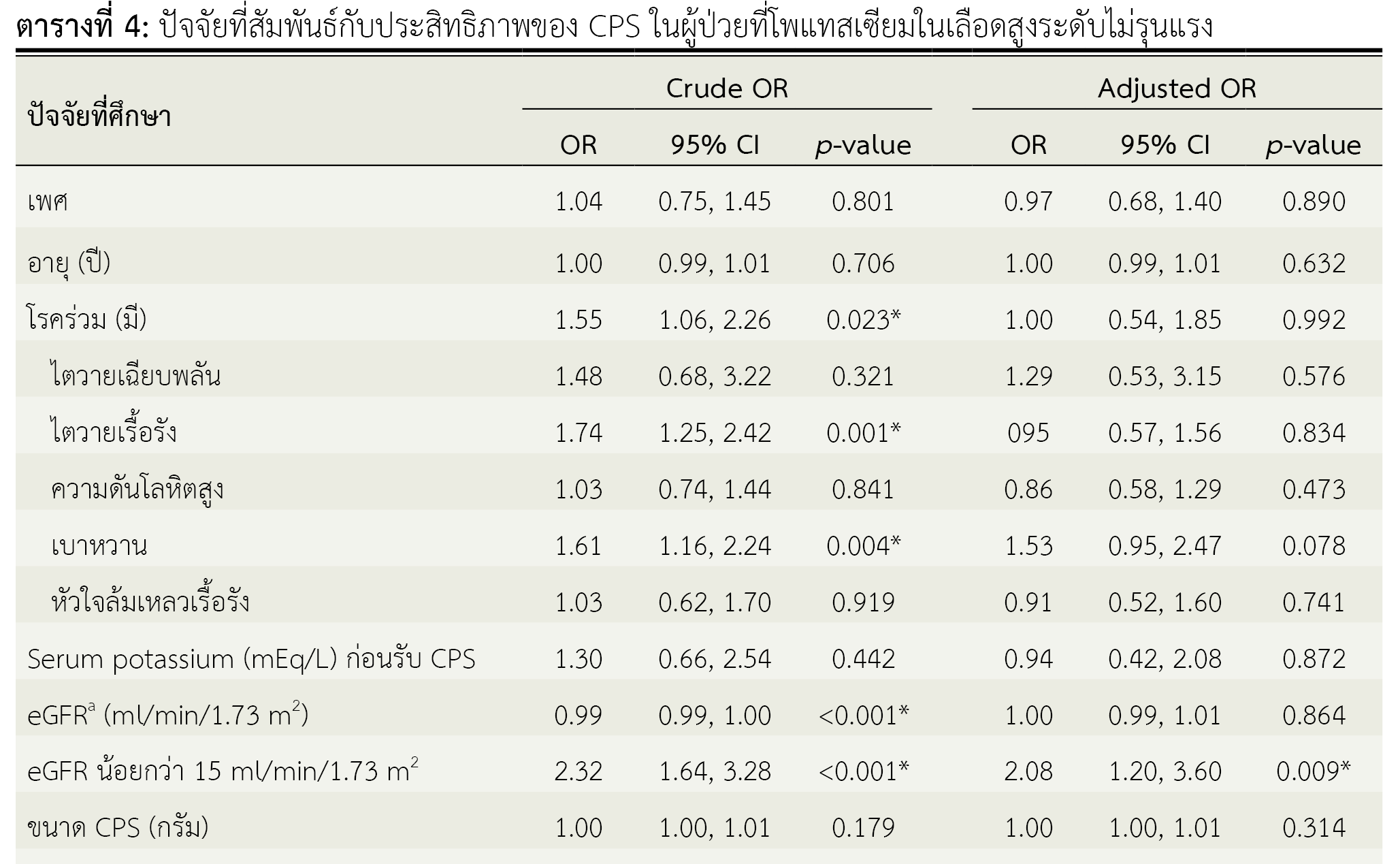
Method: This retrospective case-control study was conducted in 686 mild hyperkalemia patients who received CPS at Pattani Hospital, Thailand. We divided the subjects into two groups. The first group consisted of 475 patients whose serum potassium levels decreased to a normal range after treatment with CPS, while the second group consisted of 211 patients whose serum potassium levels did not decreased to a normal range after treatment with CPS. We compared the two groups using a t-test, Fisher’s exact test and calculated the odds ratio in logistic regression analysis.
Results: We found a statistically significant association between the efficacy of CPS and having a glomerular filtration rate (GFR) less than 15 ml/min/1.73m2 (OR 2.08, 95% CI 1.43-3.01), as well as taking spironolactone (OR 3.08, 95% CI 1.29-7.37).
Conclusion: Factors that influenced the depletion of serum potassium to normal level in mild hyperkalemia patients receiving CPS were GFR less than 15 ml/min/1.73m² and concomitant use of spironolactone.
References
Viera AJ, Wouk N. Potassium disorders: hypokalemia and hyperkalemia. Am Fam Physician. 2015;92(6):487-95. PMID: 26371733.
Flurie RW, Brophy DF. Chapter 51. Disorders of potassium and magnesium homeostasis. In: DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey L, editors. Pharmacotherapy: a pathophysiologic approach, 10th editon [Internet]. n.p.: McGraw Hill; 2017 [cited 2023 Jan 15]. Available from: https://accesspharmacy.mhmedical.com/content.aspx?bookid=1861§ionid=134127639
Kraft MD, Btaiche IF, Sacks GS, Kudsk KA. Treatment of electrolyte disorders in adult patients in the intensive care unit. Am J Health Syst Pharm. 2005;62(16):1663-82 doi: 10.2146/ajhp040300. PMID: 16085929.
นัทพล มะลิซ้อน, วีรชัย ไชยจามร. Management of water and electrolyte disorders. ใน: ดาราพร รุ้งพราย, ศยามล สุขขา, วีรชัย ไชยจามร, อุษณีย์ วนรรฆมณี, กมลวรรณ อ่อนละมัย, พิรดา วงษ์พิรา, บรรณาธิการ. คู่มือการดูแลผู้ป่วยโรคไตสำหรับเภสัชกร. พิมพ์ครั้งที่ 1. กรุงเทพฯ: ประชาชน; 2558. หน้า 127-152.
Mushiyakh Y, Dangaria H, Qavi S, Ali N, Pannone J, Tompkins D. Treatment and pathogenesis of acute hyperkalemia. J Community Hosp Intern Med Perspect. 2012;1(4):1-6. doi: 10.3402/jchimp.v1i4.7372. PMID: 23882341; PMCID: PMC3714047.
Kowa company Ltd. Kalimate [database on internet]. Tokyo: Kowa company Ltd. [cited 2023 Jun 30]. Available from: https://medical.kowa.co.jp/asset/item/18/28/7-pse_046.pdf
Yu MY, Yeo JH, Park JS, Lee CH, Kim GH. Long-term efficacy of oral calcium polystyrene sulfonate for hyperkalemia in CKD patients. PLoS One. 2017;12(3):e0173542. doi: 10.1371/journal.pone.0173542. PMID: 28328954; PMCID: PMC5362098.
Natale P, Palmer SC, Ruospo M, Saglimbene VM, Strippoli GF. Potassium binders for chronic hyperkalaemia in people with chronic kidney disease. Cochrane Database Syst Rev. 2020;6(6):CD013165. doi: 10.1002/14651858.CD013165.pub2. PMID: 32588430; PMCID: PMC7386867.
Loutradis C, Tolika P, Skodra A, Avdelidou A, Sarafidis PA. Prevalence of hyperkalemia in diabetic and non-diabetic patients with chronic kidney disease: a nested case-control study. Am J Nephrol. 2015;42(5):351-60. doi: 10.1159/000442393. PMID: 26599956.
Raebel MA. Hyperkalemia associated with use of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers. Cardiovasc Ther. 2012;30(3):e156-66. doi: 10.1111/j.1755-5922.2010.00258.x. PMID: 21883995.
Nash DM, Markle-Reid M, Brimble KS, McArthur E, Roshanov PS, Fink JC, et al. Nonsteroidal anti-inflammatory drug use and risk of acute kidney injury and hyperkalemia in older adults: a population-based study. Nephrol Dial Transplant. 2019;34(7):1145-54. doi: 10.1093/ndt/gfz062. PMID: 31264694; PMCID: PMC6603365.
Surabenjawong U, Thunpiphat N, Chatsiricharoenkul S, Monsomboon A. Prevalence of hyperkalemia in adult patients taking spironolactone and angiotensin converting enzyme inhibitors or angiotensin receptor blockers. J Med Assoc Thai. 2013;96(8):905-10. PMID: 23991595.
Tamirisa KP, Aaronson KD, Koelling TM. Spironolactone-induced renal insufficiency and hyperkalemia in patients with heart failure. Am Heart J. 2004;148(6):971-8. doi: 10.1016/j.ahj.2004.10.005. PMID: 15632880.
Liamis G, Liberopoulos E, Barkas F, Elisaf M. Diabetes mellitus and electrolyte disorders. World J Clin Cases. 2014;2(10):488-96. doi: 10.12998/wjcc.v2.i10.488.
Bengalorkar GM, Sarala N, Venkatrathnamma PN, Kumar TN. Effect of heparin and low-molecular weight heparin on serum potassium and sodium levels. J Pharmacol Pharmacother. 2011;2(4):266-9. doi: 10.4103/0976-500X.85956.
Thomas CM, Thomas J, Smeeton F, Leatherdale BF. Heparin-induced hyperkalemia. Diabetes Res Clin Pract. 2008;80(2):e7-8. doi: 10.1016/j.diabres.2008.01.019.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Health Administration Division, Office of the Permanent Secretary, Ministry of Public Health and The Society of Hospital Pharmacist, Ministry of Public Health

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
ข้อความภายในบทความที่ตีพิมพ์ในวารสารเภสัชกรรมคลินิกทั้งหมด รวมถึงรูปภาพประกอบ ตาราง เป็นลิขสิทธิ์ของกองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข การนำเนื้อหา ข้อความหรือข้อคิดเห็น รูปภาพ ตาราง ของบทความไปจัดพิมพ์เผยแพร่ในรูปแบบต่าง ๆ เพื่อใช้ประโยชน์ในเชิงพาณิชย์ ต้องได้รับอนุญาตจากกองบรรณาธิการวารสารเภสัชกรรมคลินิกอย่างเป็นลายลักษณ์อักษร
กองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข อนุญาตให้สามารถนำไฟล์บทความไปใช้ประโยชน์และเผยแพร่ต่อได้ โดยอยู่ภายใต้เงื่อนไขสัญญาอนุญาตครีเอทีฟคอมมอน (Creative Commons License: CC) โดย ต้องแสดงที่มาจากวารสาร – ไม่ใช้เพื่อการค้า – ห้ามแก้ไขดัดแปลง, Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0)
ข้อความที่ปรากฏในบทความในวารสารเป็นความคิดเห็นส่วนตัวของผู้เขียนแต่ละท่านไม่เกี่ยวข้องกับกองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข และบุคลากรในกองฯ หรือ ชมรมฯ แต่อย่างใด ความรับผิดชอบองค์ประกอบทั้งหมดของบทความแต่ละเรื่องเป็นของผู้เขียนแต่ละท่าน หากมีความผิดพลาดใด ๆ ผู้เขียนแต่ละท่านจะรับผิดชอบบทความของตนเอง ตลอดจนความรับผิดชอบด้านเนื้อหาและการตรวจร่างบทความเป็นของผู้เขียน ไม่เกี่ยวข้องกับกองบรรณาธิการ



