The Effect of Home Delivery of Medication under the COVID-19 Pandemic Situation on HIV/AIDS Treatment Outcome at Prachuap Khiri Khan Hospital
Keywords:
home delivery of medication, adherence, viral load, viral load undetectedAbstract
Background: In the situation of the COVID-19 outbreak people living with HIV/AIDS (PLHIVs) unable to receive treatment at hospital as usual. Home delivery of medication to patients is necessary to ensure that PLHIVs use medication continuously. However, treatment results should be followed up and verified after the drug is delivered to the patient.
Objective: To study the impact of home delivery of medication on medication adherence and HIV virus suppression among PLHIVs.
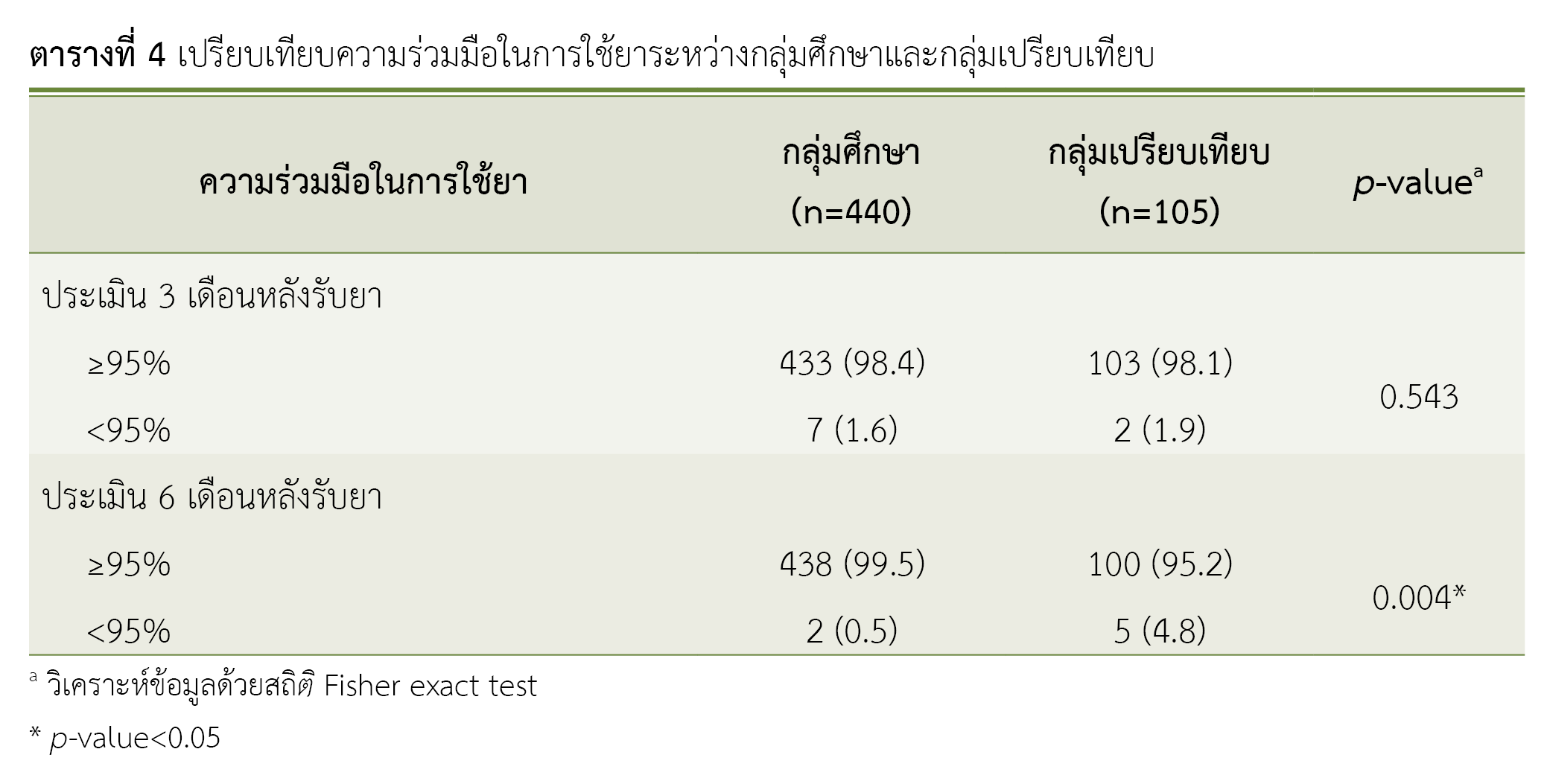
Method: This was retrospective Cohort study. The study group consisted of 440 PLHIVs who received medication by home delivery and the comparison group were 105 PLHIVs who received regular services at antiretroviral clinics. Data were collected from the medical records to compare of medication adherence and HIV virus suppression of the study group between before and after home delivery of medication and between the study group and the comparison group. Data were analyzed by statistical frequency, percentage, chi-square test, Fisher exact test and McNemar.
Results: The study group's medication adherence before and after 6 months of home delivery of medication was statistically significantly different (p=0.039), with medication adherence 6 months after receiving the medication higher than before home delivery of medication and there were 99.5% of subject in study group and 95.2% of subject in comparison group who had adherence ≥95% which was significantly difference (p<0.004). Among the study group after home delivery of medication the proportion of PLHIVs who had an undetectable viral load (<20 copies/ml) was 95.0 percent and higher than before home delivery of medication which was only 87.7 percent and statistically significant difference (p< 0.001). When compared between the study group and the comparison group it was found that there was no statistical significant difference (p=0.256).
Conclusion: PLHIVs who received the medication by home delivery had higher medication adherence 6 months after receiving the medication and proportion of undetected viral load increased.
References
Centers for Disease Control (CDC). Pneumocystis pneumonia--Los Angeles. MMWR Morb Mortal Wkly Rep. 1981;30(21):250-2. PMID: 6265753.
UNAIDS. People living with HIV [Internet]. Geneva: Joint United Nations Programme on HIV/AIDS (UNAIDS); 2014 [cited 2022 Dec 12]. Available from: https://www.unaids.org/en/resources/documents/2014/peoplelivingwithhiv
The Global Fund to Fight AIDS, Tuberculosis and Malaria. The impact of COVID-19 on HIV, TB and malaria services and systems for health: a snapshot from 502 health facilities across Africa and Asia [Internet]. Geneva: The Global Fund; 2021 [cited 2023 Jun 16]. Available from: https://reliefweb.int/attachments/043aff8c-5dc3-3be4-b9f2-fd8ecb084e4b/covid-19_2020-disruption-impact_report_en.pdf
Jewell BL, Mudimu E, Stover J, Ten Brink D, Phillips AN, Smith JA, et al. Potential effects of disruption to HIV programmes in sub-Saharan Africa caused by COVID-19: results from multiple mathematical models. Lancet HIV. 2020;7(9):e629-40. doi: 10.1016/S2352-3018(20)30211-3.
Schmittdiel JA, Karter AJ, Dyer WT, Chan J, Duru OK. Safety and effectiveness of mail order pharmacy use in diabetes. Am J Manag Care. 2013;19(11):882-7. PMID: 24511986.
Castelino S, Miah H, Auyeung V, Vogt F. Determination of the influence of home delivery of HIV therapy on virological outcomes and adherence. Int J STD AIDS. 2015;26(2):93-7. doi: 10.1177/0956462414530887.
Ridgway JP, Friedman EE, Choe J, Nguyen CT, Schuble T, Pettit NN. Impact of mail order pharmacy use and travel time to pharmacy on viral suppression among people living with HIV. AIDS Care. 2020;32(11):1372-78. doi: 10.1080/09540121.2020.1757019.
Hoke T, Bateganya M, Toyo O, Francis C, Shrestha B, Philakone P, et al. How home delivery of antiretroviral drugs ensured uninterrupted HIV treatment during COVID-19: experiences from Indonesia, Laos, Nepal, and Nigeria. Glob Health Sci Pract. 2021;9(4):978-89. doi: 10.9745/GHSP-D-21-00168.
National Institutes of Health. Office of AIDS Research. Glossary of HIV/AIDS-related terms. 9th edition [Internet]. Rockville: National Institutes of Health; 2021 [cited 2022 Dec 12]. Available from: https://clinicalinfo.hiv.gov/sites/default/files/glossary/Glossary-English_HIVinfo.pdf
ธานินทร์ ศิลป์จารุ. การวิจัยและวิเคราะห์ข้อมูลทางสถิติด้วย SPSS และ AMOS. พิมพ์ครั้งที่ 15. นนทบุรี: เอส. อาร์. พริ้นติ้ง แมสโปรดักส์; 2557.
Kvarnström K, Westerholm A, Airaksinen M, Liira H. Factors contributing to medication adherence in patients with a chronic condition: a scoping review of qualitative research. Pharmaceutics. 2021; 13(7):1100. doi: 10.3390/pharmaceutics13071100.
Nurfalah F, Yona S, Waluyo A. The relationship between HIV stigma and adherence to antiretroviral (ARV) drug therapy among women with HIV in Lampung, Indonesia. Enfermería Clínica. 2019;29(Suppl 2):234-7. doi: 10.1016/j.enfcli.2019.04.138.
Buscher A, Hartman C, Kallen MA, Giordano TP. Impact of antiretroviral dosing frequency and pill burden on adherence among newly diagnosed, antiretroviral-naive HIV patients. Int J STD AIDS. 2012;23(5):351-5. doi: 10.1258/ijsa.2011.011292.
สำนักวิชาการวิทยาศาสตร์การแพทย์. อธิบดีกรมวิทยาศาสตร์การแพทย์ เผยการเฝ้าระวังการระบาดการกลายพันธ์เชื้อโควิด-19 พบสายพันธุ์เดลต้า 76 จังหวัดในประเทศไทยแล้ว ขณะที่ กทม.พบมากถึง 95.4% [อินเทอร์เน็ต]. นนทบุรี: สำนักวิชาการวิทยาศาสตร์การแพทย์ กรมวิทยาศาสตร์การแพทย์; 2564 [สืบค้นเมื่อ 10 ก.ย. 2566]. สืบค้นจาก: https://msto.dmsc.moph.go.th/login/showimgdetil.php?id=329
Fernandes A, Brito AM, Mendes T, Alcobi A. Effect of COVID-19 pandemic on antiretroviral therapy adherence. Eur J Hosp Pharm. 2021;28(Suppl 1):A109. doi: 10.1136/ejhpharm-2021-eahpconf.224
Moyle G. The assessing patients' preferred treatments (APPT-1) study. Int J STD AIDS. 2003;14(Suppl 1):34-6. doi: 10.1258/095646203322491860.
Trotta MP, Ammassari A, Cozzi-Lepri A, Zaccarelli M, Castelli F, Narciso P, et al. Adherence to highly active antiretroviral therapy is better in patients receiving non-nucleoside reverse transcriptase inhibitor-containing regimens than in those receiving protease inhibitor-containing regimens. AIDS. 2003;17(7):1099-102. doi: 10.1097/00002030-200305020-00026.
Altice F, Evuarherhe O, Shina S, Carter G, Beaubrun AC. Adherence to HIV treatment regimens: systematic literature review and meta-analysis. Patient Prefer Adherence. 2019;13:475-90. doi: 10.2147/PPA.S192735.
Milward de Azevedo Meiners MM, Araújo Cruz I, de Toledo MI. Adherence to antiretroviral therapy and viral suppression: analysis of three periods between 2011 and 2017 at an HIV-AIDS center, Brazil. Front Pharmacol. 2023;14:1122018. doi: 10.3389/fphar.2023.1122018.
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487-97. doi: 10.1056/NEJMra050100.
ประจักร เหิกขุนทด. การพัฒนารูปแบบการดูแลรักษาผู้ติดเชื้อเอชไอวีและผู้ป่วยเอดส์ โรงพยาบาลส่องดาว. วารสารโรคเอดส์ [อินเทอร์เน็ต]. 2564 [สืบค้นเมื่อ 12 ธ.ค. 2565];33(3):151-64. สืบค้นจาก: https://he02.tci-thaijo.org/index.php/ThaiAIDSJournal/article/view/251643
Castelino S, Hurley L, Malavasi T, Oborne CA. Offering a home delivery service for HIV medication can increase patient choice. Pharmacy in Practice [Internet]. 2009 [cited 2023 Sep 10];19(1):35-8. Available from: http://www.pharmacyinpractice.com/archive/2009-volume-19-issue-1/7-PIP-Original-research-JanFeb09.pdf
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Health Administration Division, Office of the Permanent Secretary, Ministry of Public Health and The Society of Hospital Pharmacist, Ministry of Public Health

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
ข้อความภายในบทความที่ตีพิมพ์ในวารสารเภสัชกรรมคลินิกทั้งหมด รวมถึงรูปภาพประกอบ ตาราง เป็นลิขสิทธิ์ของกองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข การนำเนื้อหา ข้อความหรือข้อคิดเห็น รูปภาพ ตาราง ของบทความไปจัดพิมพ์เผยแพร่ในรูปแบบต่าง ๆ เพื่อใช้ประโยชน์ในเชิงพาณิชย์ ต้องได้รับอนุญาตจากกองบรรณาธิการวารสารเภสัชกรรมคลินิกอย่างเป็นลายลักษณ์อักษร
กองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข อนุญาตให้สามารถนำไฟล์บทความไปใช้ประโยชน์และเผยแพร่ต่อได้ โดยอยู่ภายใต้เงื่อนไขสัญญาอนุญาตครีเอทีฟคอมมอน (Creative Commons License: CC) โดย ต้องแสดงที่มาจากวารสาร – ไม่ใช้เพื่อการค้า – ห้ามแก้ไขดัดแปลง, Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0)
ข้อความที่ปรากฏในบทความในวารสารเป็นความคิดเห็นส่วนตัวของผู้เขียนแต่ละท่านไม่เกี่ยวข้องกับกองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข และบุคลากรในกองฯ หรือ ชมรมฯ แต่อย่างใด ความรับผิดชอบองค์ประกอบทั้งหมดของบทความแต่ละเรื่องเป็นของผู้เขียนแต่ละท่าน หากมีความผิดพลาดใด ๆ ผู้เขียนแต่ละท่านจะรับผิดชอบบทความของตนเอง ตลอดจนความรับผิดชอบด้านเนื้อหาและการตรวจร่างบทความเป็นของผู้เขียน ไม่เกี่ยวข้องกับกองบรรณาธิการ



