The Effect of the Estimated Glomerular Filtration Rate as a Trigger Tool Model to Prevent Vancomycin Induced Nephrotoxicity
Keywords:
vancomycin, nephrotoxicity, acute kidney injury, trigger toolAbstract
Background: Vancomycin is a broad-spectrum antimicrobial. It has bactericidal activity against Gram-positive pathogens, including Methicillin-resistant Staphylococcus aureus (MRSA) infection. Its significant adverse reaction is vancomycin induced nephrotoxicity which is a preventable drug adverse reaction. If it is detected and treated early, the kidney function can return to normal.
Objective: This study aimed to determine the effect of using estimated glomerular filtration rate (eGFR) as a Trigger tool to prevent vancomycin induced nephrotoxicity and to explore potential confounding factors that may increase the risk of nephrotoxicity in patients receiving vancomycin.
Method: This study was a retrospective study. Data were compared before and after the trial of the eGFR trigger tool system in patients receiving intravenous vancomycin for at least 48 hours in the Central Chest Institute of Thailand with a period of 1 year, during October, 2017 to September, 2019. Patients will be monitored until vancomycin is discontinued. The incidence of nephrotoxicity, defined as a decrease in eGFR by ≥25%, and/or an increase in serum creatinine (SCr) of 1.5-fold from its baseline value.
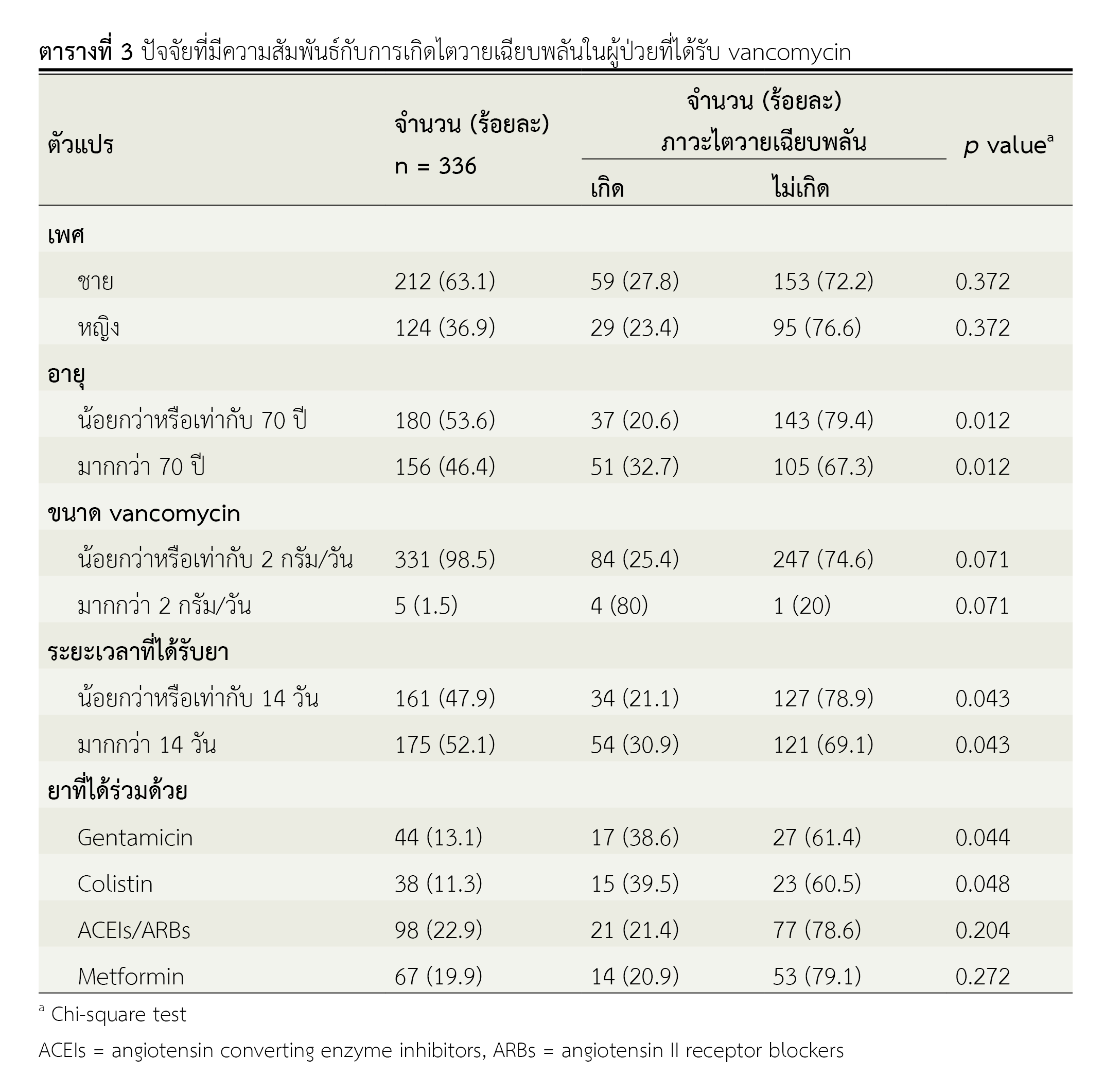
Results: A total of 366 patients were enrolled into the study. There were 157 patients in before using the eGFR trigger tool group and 179 patients in after using the eGFR trigger tool group. The study found that the incidence of acute kidney injury before and after using the eGFR trigger tool were 34.4% and 19%, respectively (p = 0.002) and the incidence of nephrotoxicity from vancomycin was significantly increased in elderly patients (>70 years), patients treated for longer than 14 days and concurrently treated with gentamycin or colistin (p = 0.012, 0.043, 0.044 and 0.048, respectively).
Conclusion: After initiation of the eGFR trigger tool, patients treated with vancomycin had a significantly lower incidence of acute renal failure than before using the eGFR trigger tool. Factors associated with vancomycin induced nephrotoxicity included patients older than 70 years, patients treated for more than 14 days, and concomitant exposure to other nephrotoxic drugs.
References
Kasmar AG, Hooper D. Pharmacology of bacterial infection: cell wall synthesis. In: Golan DE, Tashjian AH Jr, Armstrong EJ, Armstrong AW, editors. Principles of pharmacology: The pathophysiologic basis of drug therapy. 2nd ed. Baltimore: Lippincott Williams & Wilkins; 2008. p. 601-18.
Mc Evoy GK. AHFS Drug Information 2005. Bethesda, American Society of Health-System Pharmacists; 2005. p. 467-71.
Liu C, Bayer A, Cosgrove S, Daum R, Fridkin S, Gorwitz R, et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. [Internet]. 2011 [cited 2021 Dec 11];52(3):e18-e55. Available from: https://www.researchgate.net/publication/49731385
Kett DH, Cano E, Quartin AA, Mangino JE, Zervos MJ, Peyrani P, et al. Implementation of guidelines for management of possible multidrug-resistant pneumonia in intensive care: An observational, multicentre cohort study. Lancet Infect Dis. 2011;11(3):181-9.
Elyasi S, Khalili H, Dashti-Khavidaki S, Mohammadpour A. vancomycin-induced nephrotoxicity: Mechanism, incidence, risk factors and special populations. A literature review. Eur J Clin Pharmacol. 2012;68(9):1243-55
Hanrahan TP, Kotapati C, Roberts MJ, Rowland J, Lipman J, Roberts JA, et al. Factors associated with vancomycin nephrotoxicity in the critically ill. Anaesth Intensive Care. 2015;43(5):594-9
Rybak MJ, Albrecht LM, Boike SC, Chandrasekar PH. Nephrotoxicity of vancomycin, alone and with an aminoglycoside. J Antimicrob Chemother. 1990;25(4):679-87.
Rybak M, Lomaestro B, Rotschafer JC, Moellering R, Jr., Craig W, Billeter M, et al. Therapeutic monitoring of vancomycin in adult patients: A consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Am J Health Syst Pharm. 2009;66(1):82-98
Winter ME. Basic clinical pharmacokinetics. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health; 2010
Bagshaw SM, George C, Bellomo R. A comparison of the RIFLE and AKIN criteria for acute kidney injury in critically ill patients. Nephrol Dial Transplant. 2008;23(5):1569-74.
Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, et al. Acute Kidney Injury Network: Report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11(2):R31
Kellum JA, Lameire N, Aspelin P, Barsoum RS, Burdmann EA, Goldstein SL, et al. Kidney disease: Improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. 2012;2(1):1-138.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Health Administration Division, Office of the Permanent Secretary, Ministry of Public Health and The Society of Hospital Pharmacist, Ministry of Public Health

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
ข้อความภายในบทความที่ตีพิมพ์ในวารสารเภสัชกรรมคลินิกทั้งหมด รวมถึงรูปภาพประกอบ ตาราง เป็นลิขสิทธิ์ของกองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข การนำเนื้อหา ข้อความหรือข้อคิดเห็น รูปภาพ ตาราง ของบทความไปจัดพิมพ์เผยแพร่ในรูปแบบต่าง ๆ เพื่อใช้ประโยชน์ในเชิงพาณิชย์ ต้องได้รับอนุญาตจากกองบรรณาธิการวารสารเภสัชกรรมคลินิกอย่างเป็นลายลักษณ์อักษร
กองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข อนุญาตให้สามารถนำไฟล์บทความไปใช้ประโยชน์และเผยแพร่ต่อได้ โดยอยู่ภายใต้เงื่อนไขสัญญาอนุญาตครีเอทีฟคอมมอน (Creative Commons License: CC) โดย ต้องแสดงที่มาจากวารสาร – ไม่ใช้เพื่อการค้า – ห้ามแก้ไขดัดแปลง, Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0)
ข้อความที่ปรากฏในบทความในวารสารเป็นความคิดเห็นส่วนตัวของผู้เขียนแต่ละท่านไม่เกี่ยวข้องกับกองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข และบุคลากรในกองฯ หรือ ชมรมฯ แต่อย่างใด ความรับผิดชอบองค์ประกอบทั้งหมดของบทความแต่ละเรื่องเป็นของผู้เขียนแต่ละท่าน หากมีความผิดพลาดใด ๆ ผู้เขียนแต่ละท่านจะรับผิดชอบบทความของตนเอง ตลอดจนความรับผิดชอบด้านเนื้อหาและการตรวจร่างบทความเป็นของผู้เขียน ไม่เกี่ยวข้องกับกองบรรณาธิการ



