Effectiveness of a Combined Intervention to Improve Continuity of Care in Patients with Chronic Obstructive Pulmonary Diseases; a Case Study for a District Hospital in Thailand
Keywords:
chronic obstructive pulmonary disease, continuity of care, ffectiveness, combined interventionAbstract
Background: Continuity of care is one of the key factors for caring for patients with chronic obstructive pulmonary disease (COPD) in primary care.
Objectives: To evaluate clinical outcomes, quality of life and healthcare cost before and after COPD patients received a combined intervention to improve continuity of care at Paknam-Chumphon Hospital.
Methods: A quasi-experimental pre-post study was carried out at an outpatient COPD clinic of a district hospital in Thailand from May 2023 to July 2023. Adult patients with COPD who visited the COPD clinic for >6 months were eligible. The intervention consisted of 4 combined interventions; 1) multidisciplinary team reviewed and updated management of COPD patient based on GOLD guideline, 2) empowered the patients. 3) continuing care monitoring in the hospital to the community and home health care, 4) heath promotion and prevention. All patients were assessed for targeted mMRC dyspnea scale, acute exacerbation, emergency department (ER) visit, hospitalization, PEFR, FEV1, quality of life (CAT score) and healthcare cost before and after 6 months of the intervention’s implementation.
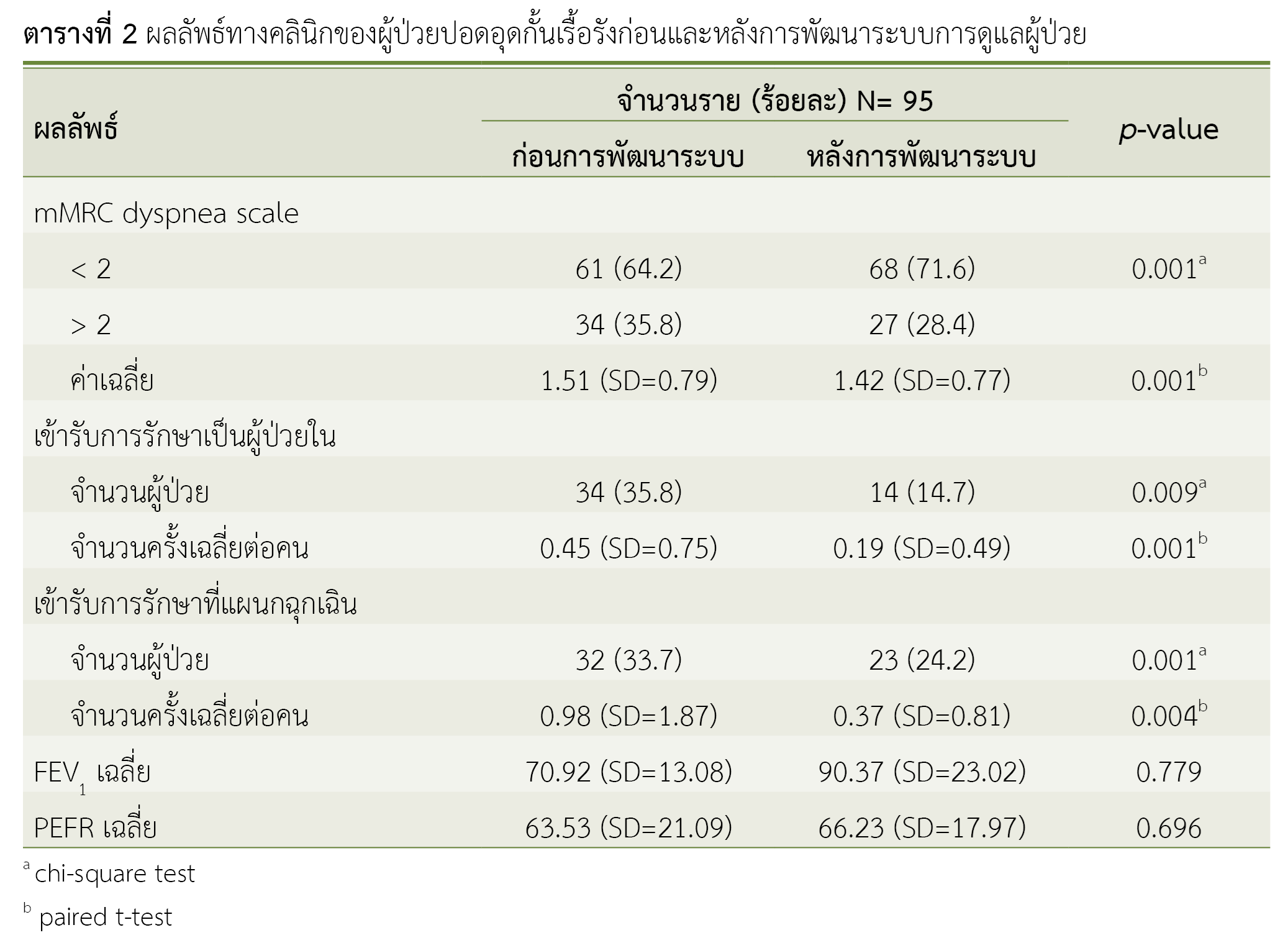
Results: A total of 95 patients were included. Most patients were male (81.1%) and average age was 66.9 years. The percentage of patients with the targeted mMRC dyspnea scale <2 increased from 64.2% to 71.6% (p<0.05) PEFR and FEV1 were increased. The acute exacerbation, number of hospitalization and ER visit were also significantly decreased (p<0.05). The percentage of patient’s quality of life defined by CAT score <10 increased from 41.1% to 65.3% (p<0.05). Total medical cost was 35.9% decreased.
Conclusions: The combined intervention to improve continuity of care has both clinical and economic benefits in patients with COPD.
References
World Health Organization. Chronic obstructive pulmonary disease (COPD) [Internet]. Geneva: WHO; 2023 [cited 2023 Feb 3]. Available from: https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd)
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Pocket guide to COPD diagnosis, management, and prevention. A guide for health care professionals. 2023 edition [Internet]. n.p.: Global Initiative for Chronic Obstructive Lung Disease, Inc.; 2023 [cited 2023 Feb 3]. Available from: https://goldcopd.org/wp-content/uploads/2023/03/POCKET-GUIDE-GOLD-2023-ver-1.2-17Feb2023_WMV.pdf
OECD. Health at a glance 2021: OECD indicators [Internet]. Paris: OECD Publishing; 2021 [cited 2023 Feb 3]. Available from: https://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-2021_ae3016b9-en
Guanais FC, Gómez-Suárez R, Pinzón L. Series of avoidable hospitalizations and strengthening primary health care: primary care effectiveness and the extent of avoidable hospitalizations in Latin America and the Caribbean [Internet]. n.p.: Inter-American Development Bank; 2012 [cited 2023 Feb 3]. Available from: https://www.researchgate.net/publication/324162719_SERIES_OF_AVOIDABLE_HOSPITALIZATIONS_AND_STRENGTHENING_PRIMARY_HEALTH_CARE_Primary_Care_Effectiveness_and_the_Extent_of_Avoidable_Hospitalizations_in_Latin_America_and_the_Caribbean
Dalal AA, Shah M, D'Souza AO, Rane P. Costs of COPD exacerbations in the emergency department and inpatient setting. Respir Med. 2011;105(3):454-60. doi: 10.1016/j.rmed.2010.09.003.
de Miguel Diez J, Carrasco Garrido P, García Carballo M, Gil de Miguel A, Rejas Gutierrez J, Bellón Cano JM, et al. Determinants and predictors of the cost of COPD in primary care: a Spanish perspective. Int J Chron Obstruct Pulmon Dis. 2008;3(4):701-12. doi: 10.2147/copd.s2427.
ภาสกร ศรีทิพย์สุโข, ประภาศรี กุลาเลิศ, อารยา ศรัทธาพุทธ, อรพรรณ โพชนุกูล, ฐิตินันท์ ไมตรี, เติมสุข รักษ์ศรีทอง, และคณะ. ต้นทุนความเจ็บป่วยการนอนโรงพยาบาลของผู้ป่วยเด็กเล็กที่มีภาวะหายใจหอบเฉียบพลันมีเสียงวี้ดโรงพยาบาลธรรมศาสตร์เฉลิมพระเกียรติ. ธรรมศาสตร์เวชสาร [อินเทอร์เน็ต]. 2559 [สืบค้นเมื่อ 3 ก.พ. 2566];16(4):553-60. สืบค้นจาก: https://asianmedjam.com/index.php/tmj/article/view/710
Rocha JVM, Marques AP, Moita B, Santana R. Direct and lost productivity costs associated with avoidable hospital admissions. BMC Health Serv Res. 2020;20(1):210. doi: 10.1186/s12913-020-5071-4.
Mulpuru S, McKay J, Ronksley PE, Thavorn K, Kobewka DM, Forster AJ. Factors contributing to high-cost hospital care for patients with COPD. Int J Chron Obstruct Pulmon Dis. 2017;12:989-995. doi: 10.2147/COPD.S126607.
Blanchette CM, Dalal AA, Mapel D. Changes in COPD demographics and costs over 20 years. J Med Econ. 2012;15(6):1176-82. doi: 10.3111/13696998.2012.713880.
Darnell K, Dwivedi AK, Weng Z, Panos RJ. Disproportionate utilization of healthcare resources among veterans with COPD: a retrospective analysis of factors associated with COPD healthcare cost. Cost Eff Resour Alloc. 2013;11:13. doi: 10.1186/1478-7547-11-13.
Kao YH, Lin WT, Chen WH, Wu SC, Tseng TS. Continuity of outpatient care and avoidable hospitalization: a systematic review. Am J Manag Care. 2019;25(4):e126-34. PMID: 30986022.
Brooke ME, Spiliopoulos N, Collins M. A review of the availability and cost effectiveness of chronic obstructive pulmonary disease (COPD) management interventions in rural Australia and New Zealand. Rural Remote Health. 2017;17(3):4017. doi: 10.22605/RRH4017.
Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175-91. doi: 10.3758/bf03193146.
Blanchette CM, Gross NJ, Altman P. Rising costs of COPD and the potential for maintenance therapy to slow the trend. Am Health Drug Benefits. 2014;7(2):98-106. PMID: 24991394; PMCID: PMC4049119.
Punekar YS, Shukla A, Müllerova H. COPD management costs according to the frequency of COPD exacerbations in UK primary care. Int J Chron Obstruct Pulmon Dis. 2014;9:65-73. doi: 10.2147/COPD.S54417.
นิกร บุญแทน. ประสิทธิภาพของการจัดตั้งคลินิกโรคหืดและปอดอุดกั้นเรื้อรังในโรงพยาบาลจอมทอง จังหวัดเชียงใหม่. วารสารสาธารณสุขล้านนา [อินเทอร์เน็ต]. 2555 [สืบค้นเมื่อ 3 ก.พ. 2566];8(1):93-108. สืบค้นจาก: https://he02.tci-thaijo.org/index.php/LPHJ/article/view/179851
สุนทรีย์ พรรษา, พนมสินธุ์ ศรีชาดา, อรุณี ศิวบวรวัฒนา, ศรายุทธ เทศรพีเมธาวีนําชัย. ผลการให้คำแนะนำเทคนิคการใช้ยาสูดพ่นโดยเภสัชกร ร่วมกับการใช้สื่อมัลติมีเดีย ในผู้ป่วยผู้ใหญ่โรคหืดและโรคปอดอุดกั้นเรื้อรัง. วารสารวิชาการสาธารณสุข [อินเทอร์เน็ต]. 2559 [สืบค้นเมื่อ 3 ก.พ. 2566];25(3):424-33. สืบค้นจาก: https://thaidj.org/index.php/JHS/article/view/273
ประภา โพธิหัง, วิสาร์กร มดทอง. ประสิทธิผลการควบคุมอาการหอบของผู้ป่วยโรคปอดอุดกันเรือรังหลังการพัฒนาระบบบริการของโรงพยาบาลในจังหวัดบุรีรัมย์. วารสารวิชาการสาธารณสุข [อินเทอร์เน็ต]. 2561 [สืบค้นเมื่อ 3 ก.พ. 2566];27(5):866-76. สืบค้นจาก: https://thaidj.org/index.php/JHS/article/view/5084
Jakovljevic MB, Lazic Z, Verhaeghe N, Jankovic S, Verhaeghe N, Annemans L. Direct medical costs of COPD diagnosis and treatment, Eastern vs. Western European country - examples of Serbia and Belgium [Internet]. Conference paper of the 9th European Health Economics; 2012 July; Zurich, Switzerland. n.p.: ResearchGate GmbH; 2012 [cited 2023 Feb 3]. Available from: https://www.researchgate.net/publication/282673515_Direct_medical_costs_of_COPD_diagnosis_and_treatment_Eastern_vs_western_European_country_-_examples_of_Serbia_and_Belgium
Dalal AA, Christensen L, Liu F, Riedel AA. Direct costs of chronic obstructive pulmonary disease among managed care patients. Int J Chron Obstruct Pulmon Dis. 2010;5:341-9. doi: 10.2147/COPD.S13771.
Rhee CK, Yoon HK, Yoo KH, Kim YS, Lee SW, Park YB, et al. Medical utilization and cost in patients with overlap syndrome of chronic obstructive pulmonary disease and asthma. COPD. 2014;11(2):163-70. doi: 10.3109/15412555.2013.831061.
Bakerly ND, Roberts JA, Thomson AR, Dyer M. The effect of COPD health forecasting on hospitalisation and health care utilisation in patients with mild-to-moderate COPD. Chron Respir Dis. 2011;8(1):5-9. doi: 10.1177/1479972310388950.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Health Administration Division, Office of the Permanent Secretary, Ministry of Public Health and The Society of Hospital Pharmacist, Ministry of Public Health

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
ข้อความภายในบทความที่ตีพิมพ์ในวารสารเภสัชกรรมคลินิกทั้งหมด รวมถึงรูปภาพประกอบ ตาราง เป็นลิขสิทธิ์ของกองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข การนำเนื้อหา ข้อความหรือข้อคิดเห็น รูปภาพ ตาราง ของบทความไปจัดพิมพ์เผยแพร่ในรูปแบบต่าง ๆ เพื่อใช้ประโยชน์ในเชิงพาณิชย์ ต้องได้รับอนุญาตจากกองบรรณาธิการวารสารเภสัชกรรมคลินิกอย่างเป็นลายลักษณ์อักษร
กองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข อนุญาตให้สามารถนำไฟล์บทความไปใช้ประโยชน์และเผยแพร่ต่อได้ โดยอยู่ภายใต้เงื่อนไขสัญญาอนุญาตครีเอทีฟคอมมอน (Creative Commons License: CC) โดย ต้องแสดงที่มาจากวารสาร – ไม่ใช้เพื่อการค้า – ห้ามแก้ไขดัดแปลง, Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0)
ข้อความที่ปรากฏในบทความในวารสารเป็นความคิดเห็นส่วนตัวของผู้เขียนแต่ละท่านไม่เกี่ยวข้องกับกองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข และบุคลากรในกองฯ หรือ ชมรมฯ แต่อย่างใด ความรับผิดชอบองค์ประกอบทั้งหมดของบทความแต่ละเรื่องเป็นของผู้เขียนแต่ละท่าน หากมีความผิดพลาดใด ๆ ผู้เขียนแต่ละท่านจะรับผิดชอบบทความของตนเอง ตลอดจนความรับผิดชอบด้านเนื้อหาและการตรวจร่างบทความเป็นของผู้เขียน ไม่เกี่ยวข้องกับกองบรรณาธิการ



