Study of the Effectiveness of Albumin Replacement in Ventilated Patients with Hypoalbuminemia at Phrae Hospital
Keywords:
hypoalbuminemia, septic shock, pneumonia, acute respiratory distress syndrome, human albuminAbstract
Background: Hypoalbuminemia can lead to acute respiratory failure and increased mortality. Various types of fluid resuscitation are used in critically ill patients, depending on their condition, and albumin is one of them. However, previous studies on albumin use in mechanically ventilated patients with hypoalbuminemia remain controversial.
Objective: To study the association between 28-day in-hospital mortality, ventilator-free days within 28 days, and hospitalization duration in ventilated patients with hypoalbuminemia, comparing those who received albumin replacement with those who did not.
Methods: This single-center retrospective cohort study included 443 mechanically ventilated patients with hypoalbuminemia (serum albumin < 2.5 g/dL) due to septic shock, pneumonia, or acute respiratory distress syndrome (ARDS), admitted to Phrae Hospital, Thailand, from January 1 to December 31, 2023. Patients either received 20% albumin or did not receive albumin. Primary outcomes were analyzed using modified Poisson regression with robust standard errors (SEs) to estimate relative risks (RRs, 95% CI). Covariates were selected from univariable logistic regression (p-value < 0.05) and directed acyclic graphs (DAGs) before fitting the final model; interaction terms were tested and multicollinearity was assessed (VIF < 5). Secondary outcomes were compared using t-tests or Wilcoxon rank sum tests.
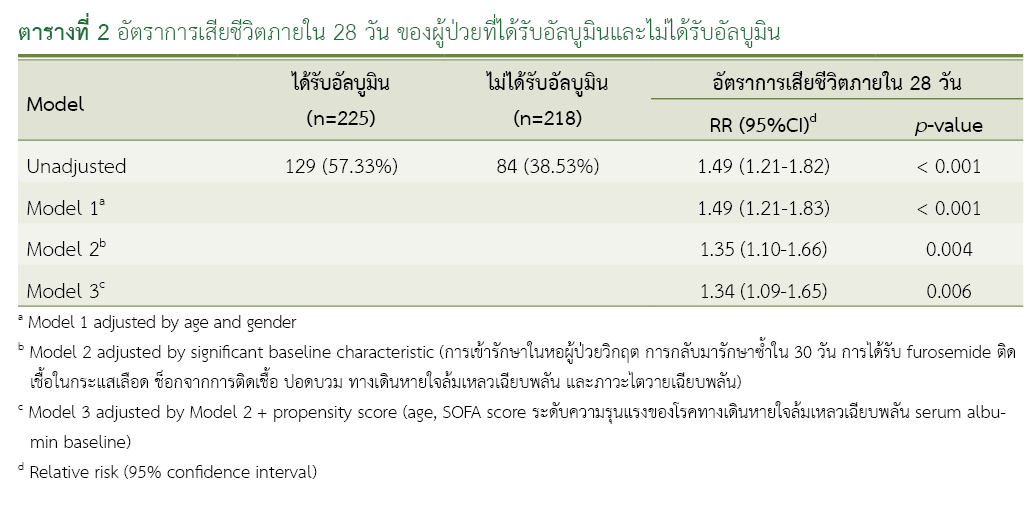
Results: Within 28 days, 129 of 225 patients (57.33%) in the albumin group and 84 of 218 patients (38.53%) in the non-albumin group had died (RR = 1.34; 95% CI: 1.09–1.65, p-value = 0.006). No statistically significant differences were observed in subgroup analyses of patients with serum albumin < 1.5 g/dL, 1.6–2.0 g/dL or SOFA score ≥ 6. However, among patients aged < 40 years in the albumin group was associated with a significantly reduced mortality rate. For secondary outcomes, ventilator-free days within 28 days were significantly lower in the albumin group (p-value < 0.001), while hospital length of stay was significantly longer compared to the non-albumin group (p-value < 0.001).
Conclusions: In mechanically ventilated patients with septic shock, pneumonia, or ARDS and hypoalbuminemia, albumin replacement, compared with no albumin use, did not improve 28-day survival.
References
Gibbs J, Cull W, Henderson W, Daley J, Hur K, Khuri SF. Preoperative serum albumin level as a predictor of operative mortality and morbidity: results from the National VA Surgical Risk Study. Arch Surg. 1999;134(1):36-42. doi: 10.1001/archsurg.134.1.36.
McNeil JB, Jackson KE, Wang C, Siew ED, Vincz AJ, Shaver CM, et al. Linear association between hypoalbuminemia and increased risk of acute respiratory distress syndrome in critically ill adults. Crit Care Explor. 2021;3(9):e0527. doi: 10.1097/CCE.0000000000000527.
Alexander MR, Stumpf JL, Nostrant TT, Khanderia U, Eckhauser FE, Colvin CL. Albumin utilization in a university hospital. DICP. 1989;23(3):214-7. doi: 10.1177/106002808902300304.
Tarín Remohí MJ, Sánchez Arcos A, Santos Ramos B, Bautista Paloma J, Guerrero Aznar MD. Costs related to inappropriate use of albumin in Spain. Ann Pharmacother. 2000;34(10):1198-205. doi: 10.1345/aph.19385.
Debrix I, Combeau D, Stephan F, Benomar A, Becker A. Clinical practice guidelines for the use of albumin: results of a drug use evaluation in a Paris hospital. Tenon Hospital Paris. Pharm World Sci. 1999;21(1):11-6. doi: 10.1023/a:1008635005398.
Cochrane Injuries Group Albumin Reviewers. Human albumin administration in critically ill patients: systematic review of randomised controlled trials. BMJ. 1998;317(7153):235-40. doi: 10.1136/bmj.317.7153.235.
Wilkes MM, Navickis RJ. Patient survival after human albumin administration: a meta-analysis of randomized controlled trials. Ann Intern Med. 2001;135(3):149-64. doi:10.7326/0003-4819-135-3-200108070-00007.
Foley EF, Borlase BC, Dzik WH, Bistrian BR, Benotti PN. Albumin supplementation in the critically ill: a prospective, randomized trial. Arch Surg. 1990;125(6):739-42. doi: 10.1001/archsurg.1990.01410180063012.
Tseng CH, Chen TT, Wu MY, Chan MC, Shih MC, Tu YK. Resuscitation fluid types in sepsis, surgical, and trauma patients: a systematic review and sequential network meta-analyses. Crit Care. 2020;24(1):693. doi: 10.1186/s13054-020-03419-y.
Wang X, Zhang T, Gao X, Cai H, Guo M, Liu Q, et al. Early human albumin administration is associated with reduced mortality in septic shock patients with acute respiratory distress syndrome: a retrospective study from the MIMIC-III database. Front Physiol. 2023;14:1142329. doi: 10.3389/fphys.2023.1142329.
Annane D, Siami S, Jaber S, Martin C, Elatrous S, Descorps Declère A, et al. Effects of fluid resuscitation with colloids vs crystalloids on mortality in critically ill patients presenting with hypovolemic shock: the CRISTAL randomized trial. JAMA. 2013;310(17):1809-17. doi: 10.1001/jama.2013.280502.
Caironi P, Tognoni G, Masson S, Fumagalli R, Pesenti A, Romero M, et al. Albumin replacement in patients with severe sepsis or septic shock. N Engl J Med. 2014;370(15):1412-21. doi: 10.1056/NEJMoa1305727.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Health Administration Division, Office of the Permanent Secretary, Ministry of Public Health and The Society of Hospital Pharmacist, Ministry of Public Health

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
ข้อความภายในบทความที่ตีพิมพ์ในวารสารเภสัชกรรมคลินิกทั้งหมด รวมถึงรูปภาพประกอบ ตาราง เป็นลิขสิทธิ์ของกองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข การนำเนื้อหา ข้อความหรือข้อคิดเห็น รูปภาพ ตาราง ของบทความไปจัดพิมพ์เผยแพร่ในรูปแบบต่าง ๆ เพื่อใช้ประโยชน์ในเชิงพาณิชย์ ต้องได้รับอนุญาตจากกองบรรณาธิการวารสารเภสัชกรรมคลินิกอย่างเป็นลายลักษณ์อักษร
กองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข อนุญาตให้สามารถนำไฟล์บทความไปใช้ประโยชน์และเผยแพร่ต่อได้ โดยอยู่ภายใต้เงื่อนไขสัญญาอนุญาตครีเอทีฟคอมมอน (Creative Commons License: CC) โดย ต้องแสดงที่มาจากวารสาร – ไม่ใช้เพื่อการค้า – ห้ามแก้ไขดัดแปลง, Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0)
ข้อความที่ปรากฏในบทความในวารสารเป็นความคิดเห็นส่วนตัวของผู้เขียนแต่ละท่านไม่เกี่ยวข้องกับกองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข และบุคลากรในกองฯ หรือ ชมรมฯ แต่อย่างใด ความรับผิดชอบองค์ประกอบทั้งหมดของบทความแต่ละเรื่องเป็นของผู้เขียนแต่ละท่าน หากมีความผิดพลาดใด ๆ ผู้เขียนแต่ละท่านจะรับผิดชอบบทความของตนเอง ตลอดจนความรับผิดชอบด้านเนื้อหาและการตรวจร่างบทความเป็นของผู้เขียน ไม่เกี่ยวข้องกับกองบรรณาธิการ



