EFFECTS OF THE “LONG Time DO” PROGRAM TO ENHANCE SELF-EFFICACY WITH SOCIAL SUPPORT FOR HEALTH BEHAVIORS MODIFICATION IN ABDOMINAL OBESITY AMONG HEALTH PERSONNEL
Keywords:
Abdominal obesity, Health behaviors, Self-efficacy, Social supportAbstract
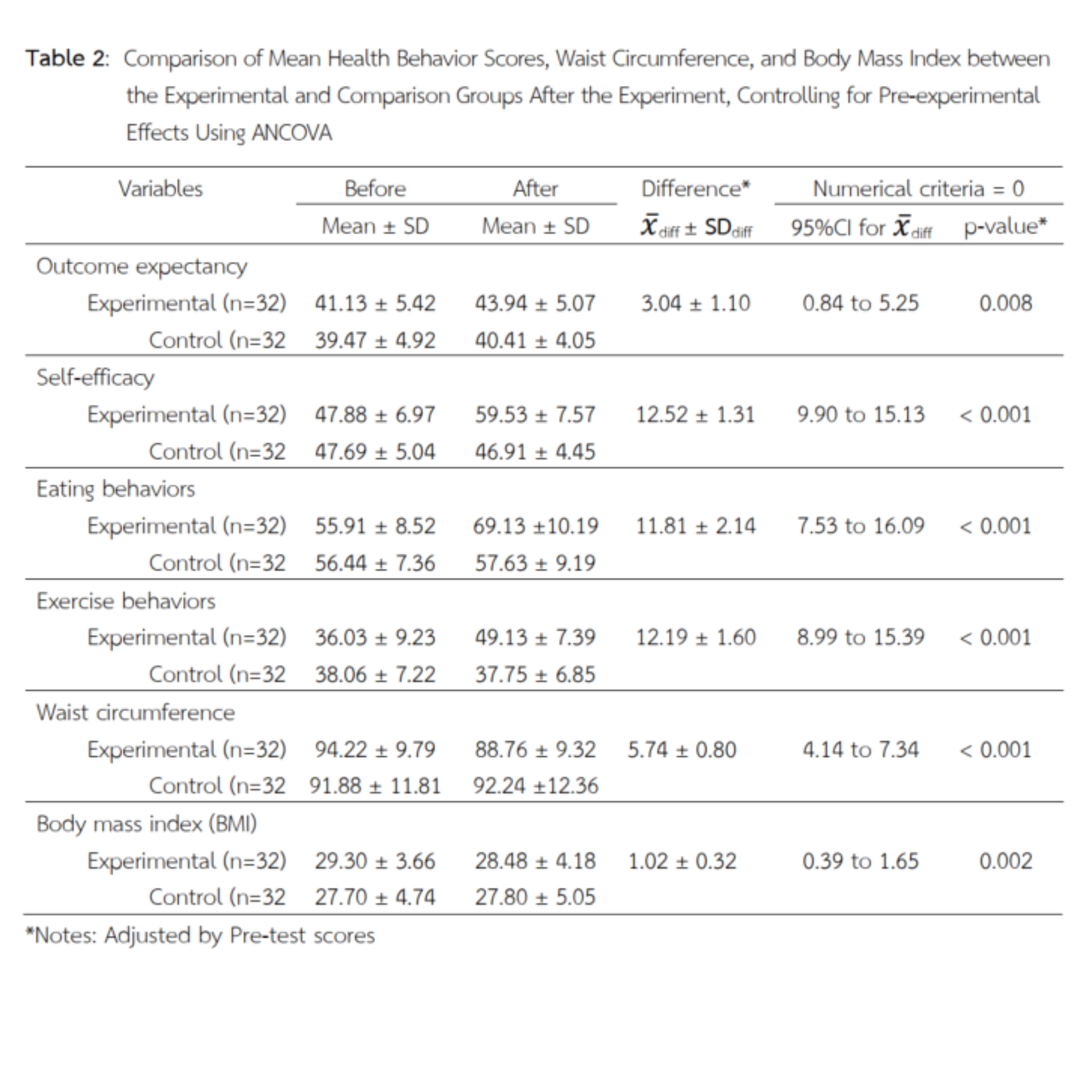
Central obesity among healthcare personnel is a significant issue that impacts not only their personal health but also their credibility as role models for the public. This quasi-experimental research aimed to evaluate the effectiveness of the “LONG Time DO” program, designed to enhance self-efficacy and social support for health behavior modification among healthcare personnel with central obesity. The sample consisted of 64 healthcare personnel diagnosed with central obesity, divided into an experimental group (n=32), which participated in the 12-week program, and a comparison group (n=32), which received standard care. Data were collected at baseline and post-intervention using health behavior questionnaires and physical assessments. Statistical analyses employed descriptive statistics, Chi-square test, Independent t-test, Paired t-test, and ANCOVA. The results revealed that, post-intervention, the experimental group had significantly higher mean scores than the comparison group in outcome expectation (X̅diff = 3.04, 95% CI: 0.84 to 5.25), self-efficacy (X̅diff = 12.52, 95% CI: 9.90 to 15.13), eating behavior (X̅diff = 11.81, 95% CI: 7.53 to 16.09), and exercise behavior (X̅diff = 12.19, 95% CI: 8.99 to 15.39). Furthermore, the experimental group demonstrated a significant reduction in waist circumference (X̅diff = 5.74, 95% CI: 4.14 to 7.34) and Body Mass Index (X̅diff = 1.02, 95% CI: 0.39 to 1.65). Within-group comparisons indicated significant improvements in all variables for the experimental group, whereas the comparison group showed no significant changes. These findings suggest that the “LONG Time DO” program is effective and can be applied to develop health interventions aimed at reducing central obesity among healthcare personnel on a wider scale.
References
Annesi J. J. & Mareno N. (2015). Improvement in emotional eating associated with an enhanced body image in obese women: mediation by weight-management treatments’ effects on self-efficacy to resist emotional cues to eating. Journal of Advanced Nursing, 71(12), 2923-2935. https://doi.org/10.1111/jan.12766
Bandura, A. (1997). Self-efficacy: The exercise of control. W H Freeman/Times Books/ Henry Holt & Co.
Best, J.W. (1981). Research in Education. New Jersey: Prentice-Hall.
Boongird, P. (2017). Impact of physical activity and diet on the development of dementia, chronic kidney disease, diabetes and cardiovascular disease in a Thai general population in Ubon Ratchathani. Health Systems Research Institute [HSRI].
Boontein P. et al. (2017). Factors related to Metabolic Syndrome among Patients at Out-patient Department. Journal of Nursing Science, 35(4), 74–86.
Bueng Kan Provincial Public Health Office. (2024). Report on waist circumference and body mass index screening results for public health personnel in Bueng Kan Province for the year 2024.
Chirawatkul, A. (2013). Statistics for health science research (3rd ed.). Bangkok: Wittayapat.
Dissara W. & Rueangphut P. (2020). The effect of isotonic exercise program to health status of health Volunteers in community. Journal of MCU Nakhondhat, 7(6), 207-216.
Ekaplakorn, W. (Ed.). (2021). The 6th Thai National Health Examination Survey (NHES VI) B.E. 2019 - 2022] (1st ed.). Faculty of Medicine Ramathibodi Hospital, Mahidol University.
Health Systems Research Institute. (2018). Handbook of guidelines for managing abdominal obesity and its complications. www.https://kb.hsri.or.th/dspace/handle/11228/4932?locale-attribute=th
Heris, M. A. (2017). A Comparison between LEARN Program and Cognitive-Behavior Intervention on Modifying Leptin Levels, Body Mass Index, Eating, Exercise and Self-Efficacy among Obese and Overweight Women. International Journal of Applied Behavioral Sciences, 4(4), 11-21.
House, J. S. (1981). Work stress and social support. California: Addison-Wesley.
Jaiyod N. & Manoton A. (2023). Effectiveness of applying the concept of health belief model in modifying obesity reduction behavior of Sukhothai personal, Muang district, Sukhothai province. Academic Journal of Community Public Health, 9(1), 54-68.
Khongphianthum O. et al. (2016). Effects of Self – Regulation Program on Hula Hoop Exercise, Dietary Control and Waist Circumference among Central Obesity Health Volunteers. The Journal of Faculty of Nursing Burapha University, 24(4), 77-88.
Ministry of Public Health. (2024). Health Data Center [HDC]. https://hdc.moph.go.th/center/public/main
Mueang Bueng Kan District Public Health Office. (2024). Preliminary health status report of public health personnel in Mueang Bueng Kan District, 2024. [Unpublished report].
Ninphupataweechot S. et al. (2021). The Metabolic Syndrome among Health Care Providers in Fort Hospital, Udonthani Province. Udonthani Hospital Medical Journal, 29(1), 61–69.
Palapol T. et al. (2017). The Effect of Enhancing Perceived Self-Efficacy Program on Food Consumption and Exercise Behavior in Adults at Risk for Metabolic Syndrome. Journal of Nursing Science Chulalongkorn University, 29(1), 81-91.
Srimongnam V. & Peanchana A. (2015). The Effects of a Dietary Program by Modification Self-Efficacy Theory the Implement to Stages of Change Model and Social Support Theory for Nursing Students with Overweight of Ratchathani University. Ratchathani Journal, 13(2), 115–123.
Supruang J. et al. (2021). Predicting factors of health promoting behaviors among working-age adults with metabolic syndrome. Journal of Social Science and Buddhistic Anthropology, 6(8), 387- 399
Threerapongphatthana, P. (2023). The factors predicting body mass index over the normal range of staff in buddhachinaraj phitsanulok hospital. Department of health Service Support Journal, 17(3), 27–36.
Wongmusik P. et al. (2015). Effects of Weight Control Program by Application of the Motivation Theory and Social Support for Body Mass Index, Waist Circumference Knowledge and Weight Control Behaviors of Staffs in fort Wiphavadlrangsit Hospital. Journal of The Royal Thai Army Nurses, 16(1), 33-40.
World Health Organization. (2023). One billion people globally estimated to be living with obesity by 2030. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
Wutthitham N. et al. (2023). Intermittent Fasting and Adequate Protein Consumption for Obesity or Overweight Prevention: A Systematic Review. Nursing Journal CMU, 50(4), 239-251.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Primary Health Care Journal (Northeastern Edition)

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.



