FACTORS INFLUENCING DEPRESSION AMONG LATE ADOLESCENTS AFTER THE COVID-19 PANDEMIC: A CROSS-SECTIONAL STUDY IN KLAENG DISTRICT, RAYONG, THAILAND
Keywords:
Depression, Resilience, Pandemic fatigue, Cyberbullying, Late adolescentsAbstract
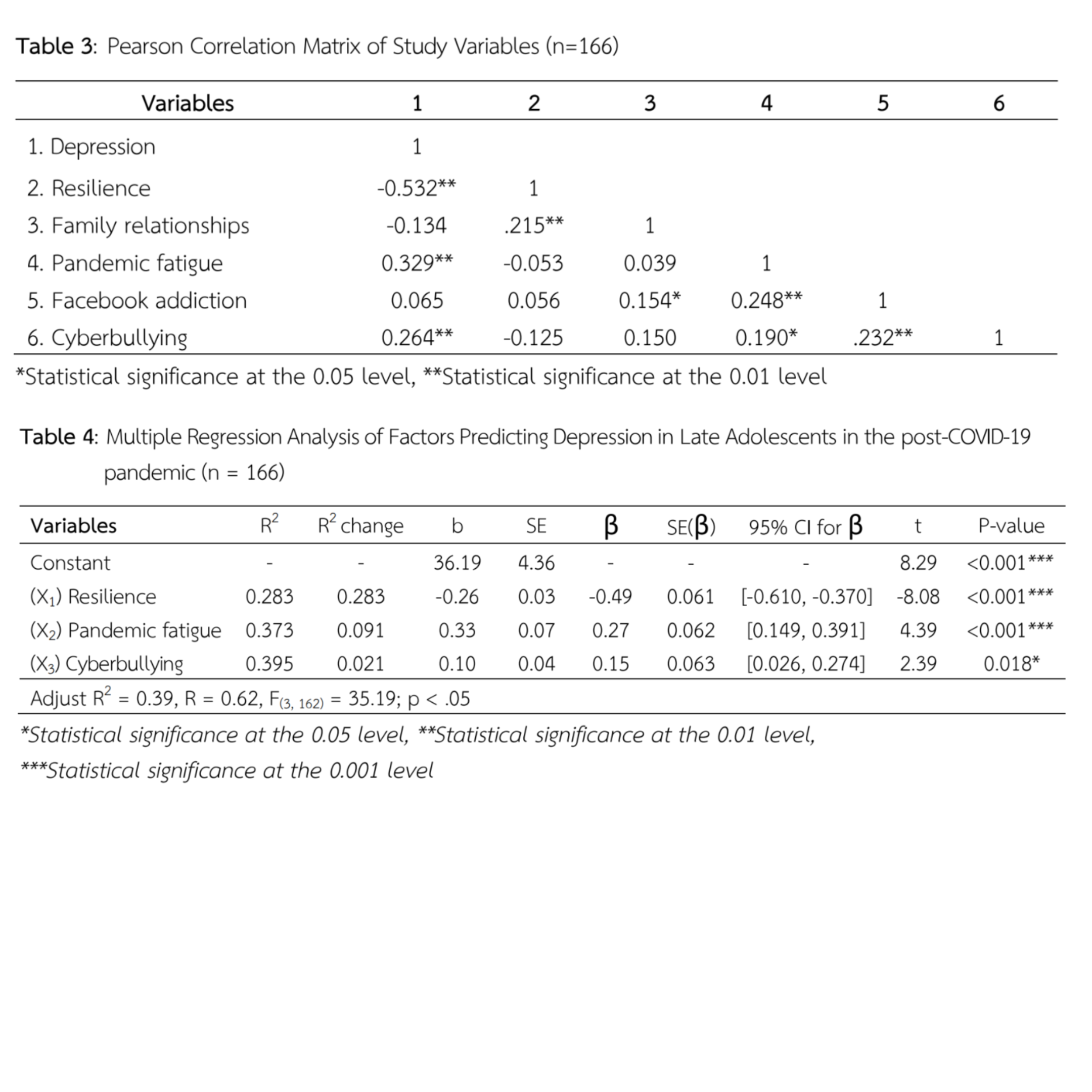
Depression is a prevalent mental health issue among late adolescents in the post-COVID-19 era, driven by the necessity for adaptation and significant lifestyle changes. Understanding the factors associated with depression is crucial for developing effective prevention strategies. This cross-sectional descriptive study aimed to investigate depression and its influencing factors among late adolescents in Klaeng District, Rayong Province. A sample of 166 participants was selected using stratified random sampling. Data collection was conducted via questionnaires between August and September 2022. Data were analyzed using descriptive statistics and stepwise multiple regression analysis. The results revealed that 63.86% of late adolescents experienced depression, classified as mild to moderate (22.29%) and severe (41.57%). Factors significantly influencing depression included resilience (β = -0.49, 95% CI [-0.610, -0.370]), pandemic fatigue (β = 0.27, 95% CI [0.149, 0.391]), and cyberbullying (β = 0.15, 95% CI [0.026, 0.274]). Together, these factors accounted for 39.50% of the variance in depression (R2 = 0.395, F = 35.72, p < 0.001). These findings indicate a relatively high prevalence of depression among late adolescents following the COVID-19 pandemic. Resilience served as a protective psychological factor, whereas pandemic fatigue and cyberbullying were identified as significant risk factors associated with depression. Therefore, healthcare professionals overseeing the mental health of this demographic should implement regular depression screening. Furthermore, interventions aimed at promoting resilience, mitigating pandemic fatigue, and reducing cyberbullying should be prioritized to effectively prevent depression in late adolescents.
References
Aknin L. B. et al. (2022). Mental health during the first year of the COVID-19 pandemic: A review and recommendations for moving forward. Perspectives on Psychological Science, 17(4), 915–936. https://doi.org/10.1177/17456916211029964
Alexander J. M. et al. (2022). Increased severity of mental health symptoms among adolescent inpatients during COVID-19. General Hospital Psychiatry, 77(2022), 77–79. https://doi.org/10.1016/j.genhosppsych.2022.04.004
Alrajeh S. M. et al. (2021). An investigation of the relationship between cyberbullying, cybervictimization, and depression symptoms: A cross-sectional study among university students in Qatar. PLoS ONE, 16(12), e0260263. https://doi.org/10.1371/journal.pone.0260263
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders: DSM-5-TR. American Psychiatric Association.
Andreassen C. S. et al. (2012). Development of a Facebook addiction scale. Psychological Reports, 110(2), 501-517. https://doi.org/10.2466/02.09.18.PR0.110.2.501-517
Blachnio A. & Przepiorka A. (2015). Internet use, Facebook intrusion, and depression: Results of a cross-sectional study. European Psychiatry, 30(6), 681-684. https://doi.org/10.1016/j.eurpsy.2015.04.002
Chen L. et al. (2023). Anxiety, depression symptoms, and psychological resilience among hospitalized COVID‐19 patients in isolation: A study from Wuhan, China. Brain and Behavior, 13(12), e3274. https://doi.org/10.1002/brb3.3274
Chotpitayasunondh V. & Dhammapeera P. (2021). Study of the effects of pandemic fatigue on mental health problems under the situation of the COVID-19 pandemic in university students. Bureau of Mental Health Academics, Department of Mental Health, Ministry of Public Health.
Christoph P. et al. (2022). The impact of migration status on adolescents’ mental health during COVID-19. Healthcare, 10(1), 176. https://doi.org/10.3390/healthcare10010176
Cohen, J. (1992). A power primer. Psychological Bulletin, 112(1), 155–59. https://doi.org/10.1037/0033-2909.112.1.155
Czeisler M. É. et al. (2021). Mental health, substance use, and suicidal ideation during the COVID-19 pandemic-United States, June 24–30, 2020. Morbidity and Mortality Weekly Report, 69(32), 1049–1057. https://doi.org/10.15585/mmwr.mm6932a1
Damdee W. et al. (2021). Relationships of cyberbullying with depression and aggressive behaviors among adolescents in a province of the central region. The Journal of Psychiatric Nursing and Mental Health, 35(1), 78–90.
Do H. K. et al. (2022). Sleep and mental health among adolescents during the COVID-19 pandemic. Psychiatry Investigation, 19(8), 637-645. https://doi.org/10.30773/pi.2021.0342
Doane A. N. et al. (2013). Development of the cyberbullying experiences survey. Emerging Adulthood, 1(3), 207–218. https://doi.org/10.1177/2167696813479584
Grotberg, E. H. (1995). A guide to promoting resilience in children: Strengthening the human spirit (Vol. 8). The Hague, Netherlands: Bernard van Leer Foundation.
Gruber J. et al. (2020). Mental health and clinical psychological science in the time of COVID-19: Challenges, opportunities, and a call to action. American Psychologist, 76(3), 409-426. https://doi.org/10.1037/amp0000707
Ho, T. T. Q. (2021). Facebook addiction and depression: Loneliness as a moderator and poor sleep quality as a mediator. Telematics and Informatics, 61, e101617. https://doi.org/10.1016/j.tele.2021.101617
Janjadkarn B. et al. (2019). Predictive factors of depression among high school students in the municipality of Chantaburi. Journal of Phrapokklao Nursing College, 30(2), 62-75.
Kumar A. & Nayar K. R. (2021). COVID-19 and its mental health consequences. Journal of Mental Health, 30(1), 1-2. https://doi.org/10.1080/09638237.2020.1757052
Lilleholt L. et al. (2020). Pandemic fatigue: Measurement, correlates, and consequences. PsyArXiv.
Liu Z. et al. (2024). Reciprocal relationship between resilience and depression: A 3-year longitudinal study during the COVID-19 pandemic. Current Psychology, 43(12), 11343-11351. https://doi.org/10.1007/s12144-023-05210-y
Maneenil A. et al. (2022). Factors influencing depression of late adolescents. Journal of Nursing and Health Research, 38(1), 293-307.
Mathur M. et al. (2023). Family stress during the COVID-19 pandemic: A qualitative analysis. BMJ Open, 13(e061396), 1-7. https://doi.org/10.1136/bmjopen-2022-061396
Morrison-Valfre, M. (2021). Foundations of mental health care (7th ed.). Elsevier.
Nintachan, P. (2015). Resilience: Concept, assessment, and application. Bangkok: Judthong.
Nomura K. et al. (2021). Cross-sectional survey of depressive symptoms and suicide-related ideation at a Japanese national university during the COVID-19 stay-home order. Environmental Health and Preventive Medicine, 26(30), 1-9. https://doi.org/10.1186/s12199-021-00953-1
Pfefferbaum B. & North C. S. (2020). Mental health and the COVID-19 pandemic. New England journal of medicine, 383(6), 510-512. https://doi.org/10.1056/NEJMp2008017
Phanasathit M. et al. (2015). Validity of the Thai version of the Bergen Facebook Addiction Scale (Thai-BFAS). Journal of the Medical Association of Thailand, 98(2), S108–S117.
Phaowiriya H. et al. (2021). Cyberbullying behavior and cybervictimization among nursing students. Nursing Journal, 48(1), 159–173.
Racine N. et al. (2021). Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: A meta-analysis. JAMA Pediatrics, 175(11), 1142-1150. https://doi.org/10.1001/jamapediatrics.2021.2482
Radloff, L. S. (1997). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385-401.
Rajanagarindra Institute of Child and Adolescent Mental Health, Department of Mental Health. (2018). Guidelines for the care of adolescents with depression. Bangkok: Beyond Publishing.
Ruksee N. et al. (2021). A study of the stress, anxiety, and family relationships among Thai people after the COVID-19 pandemic in the early stages. Quality of Life and Law Journal, 17(1), 94-108.
Secondary Educational Service Area Office Chonburi Rayong. (2022). Summary of educational information: Data Management Center (DMC 65). Group of Policy and Planning, Secondary Educational Service Area Office Chonburi Rayong.
Srisatitanarakul, B. (2010). Sample size determination and adjustment for anticipated data loss. Journal of Nursing Research, 18(1), 45–52.
Steinberg, L. (2022). Adolescence (13th ed.). McGraw-Hill.
Sukonit, P. (2015). Concepts of psychiatric disorders. In M. Lortarakul & P. Sukonit (Eds.), Ramathibodi Psychiatry Textbook (4th ed.). Department of Psychiatry, Faculty of Medicine Ramathibodi Hospital.
Thongpradab J. et al. (2019). The relationships among Facebook addiction, self-esteem, and depression in high school students. Thai Red Cross Nursing Journal, 12(2), 116-133.
Trangkhasombat M. et al. (1997). The use of CES-D in screening for depression in adolescents. Journal of the Psychiatric Association of Thailand, 42(1), 168–170.
Waldmann T. et al. (2023). The cost-utility of an intervention for children and adolescents with a parent having a mental illness in the framework of the German health and social care system: a health economic evaluation of a randomized controlled trial. Child and Adolescent Psychiatry and Mental Health, 17(2023), 141. https://doi.org/10.1186/s13034-023-00693-w
Watanapanyasakul, R. (2021). Relational ethics factor influencing depressive symptoms among adolescents, Srinakharinwirot Prasarnmit. Journal of Psychiatric Association Thailand, 66(4), 417-428.
World Health Organization. (2023). Advice for the public: Coronavirus disease (COVID-19). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public
World Health Organization. (2024). Thailand COVID-19 situation report. https://www.who.int/thailand/news/detail/19-02-2024-the-situation-report-on-covid19
Wu Q. et al. (2024). Pandemic fatigue and depressive symptoms among college students in the COVID-19 context: Indirect effects through sense of control and intolerance of uncertainty. BMC Psychology, 12, 21. https://doi.org/10.1186/s40359-024-01521-2
Zhou J. et al. (2020). Prevalence of depression and its correlative factors among female adolescents in China during the coronavirus disease 2019 outbreak. Globalization and Health, 16(2020), 69. https://doi.org/10.1186/s12992-020-00601-3
Zuckerman, M. (1999). Diathesis-stress models. In M. Zuckerman, Vulnerability to psychopathology: A biosocial model. American Psychological Association.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Primary Health Care Journal (Northeastern Edition)

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.



