Evaluation of the Appropriateness of Prescribing Direct Oral Anticoagulants at Songkhla Hospital
Keywords:
direct oral anticoagulants, DOACs, adverse drug reactionsAbstract
Background: A review of adverse drug reactions from the use of direct oral anticoagulants (DOACs) between 2021 and 2022 at Songkhla Hospital revealed two cases of grade I adverse events, including death, necessitating the use of expensive antidotes, thereby impacting both patient lives and drug costs.
Objective: To evaluate the appropriateness of prescribing DOACs and to assess the incidence of adverse drug reactions.
Method: This was a retrospective descriptive study that collected data from electronic databases and patient medical records from October 1, 2022, to September 30, 2023.
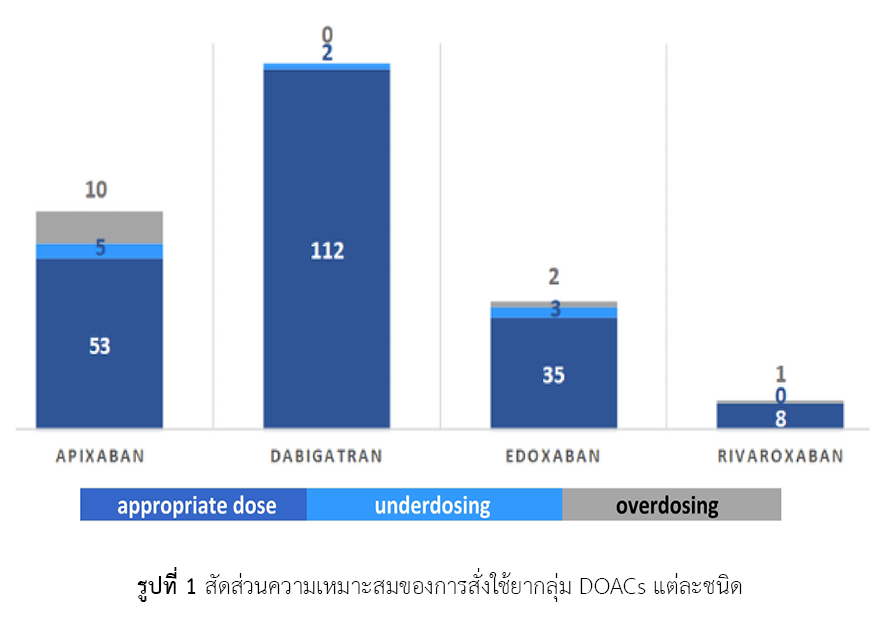
Result: A total of 231 prescriptions were reviewed, with 208 (90.04%) being for appropriate doses and 23 (9.96%) for inappropriate doses. Among the inappropriate doses, 10 (4.33%) were underdosed, and 13 (5.63%) were overdosed. Adverse drug reactions were reported in 7 (3.03%) of the appropriately dosed patients, including 6 bleeding events (2.60%) and 1 case of swollen feet (0.43%). One bleeding event (0.43%) was reported in a patient who received an inappropriately dosed medication. Patients with inappropriate doses had 1.29-fold higher odds of experiencing adverse drug reactions compared to those with appropriate doses (OR = 1.29, 95%CI: 0.15 – 10.97).
Conclusion: Our study found that inappropriate prescribing of DOACs was associated with a 29% increased risk of adverse drug reactions compared to appropriate prescribing. While this finding did not reach statistical significance due to limitations in reported data, the small sample size, and the short observation period, it was a crucial reminder for physicians to be more aware when prescribing these medications.
References
Barra ME, Fanikos J, Connors JM, Sylvester KW, Piazza G, Goldhaber SZ. Evaluation of dose-reduced direct oral anticoagulant therapy. AM J Med. 2016;129(11):1198-204. doi: 10.1016/j.amjmed.2016.05.041.
ชาริณี มีอาษา, ไชยสิทธิ์ วงศ์วิภาพร, ชญานิศ น่าชม, สุปราณี สิงหพีระกุล, ผันสุ ชุมวรฐายี, วีรวรรณ อุชายภิชาติ. การทบทวนรูปแบบและความเหมาะสมของขนาดยาต้านการแข็งตัวของเลือดชนิดรับประทานกลุ่มใหม่ในผู้ป่วยนอก ณ โรงพยาบาลศรีนครินทร์. ศรีนครินทร์เวชสาร [อินเทอร์เน็ต]. 2561 [สืบค้นเมื่อ 12 เม.ย. 2567];33(5 suppl):114-24. สืบค้นจาก: https://thaidj.org/index.php/smnj/article/view/4127
Navar AM, Kolkailah AA, Overton R, Shah NP, Rousseau JF, Flaker GC, et al. Trends in oral anticoagulant use among 436 864 patients with atrial fibrillation in community practice, 2011 to 2020. J Am Heart Assoc. 2022;11(22):e026723. doi: 10.1161/JAHA.122.026723.
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373-498. doi: 10.1093/eurheartj/ehaa612.
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37(38):2893-962. doi: 10.1093/eurheartj/ehw210.
Davis C. Drug information for the healthcare professional. 15th ed. Philadelphia: Lippincott Williams & Wilkins; 2022.
MICROMEDEX® DRUGDEX®. Apixaban, Rivaroxaban, Edoxaban, Dabigatran. In: MICROMEDEX® DRUGDEX® System [Database on the internet]. Colorado: Thomson Reuters (Healthcare); 2024 [cited 2024 Apr 12]. Available from: https://www.thomsonhc.com [Subscription required to view]
Chen A, Stecker E, A Warden B. Direct oral anticoagulant use: a practical guide to common clinical challenges. J Am Heart Assoc. 2020;9(13):e017559. doi: 10.1161/JAHA.120.017559.
Pongsathabordee C, Saringkarn P, Ratanapornsompong K, Rungruang R, Srithonrat S, Tangkaotong P, et al. Appropriateness of direct oral anticoagulant dosing in patients with atrial fibrillation at a tertiary care hospital in Thailand. Explor Res Clin Soc Pharm. 2024;16:100507. doi: 10.1016/j.rcsop.2024.100507.
พรวลัย บุญเมือง, บรรณาธิการ. Transition of anticoagulant. หนังสือประกอบการประชุมโครงการอบรมหลักสูตรการบริบาลทางเภสัชกรรมในผู้ป่วยโรคหลอดเลือดสมอง; 4-5 เม.ย. 2567; สถาบันประสาทวิทยา. กรุงเทพมหานคร: มหาวิทยาลัยมหิดล; 2567.
Poli D, Antonucci E, Ageno W, Berteotti M, Falanga A, Pengo V, et al. Inappropriate underdosing of direct oral anticoagulants in atrial fibrillation patients: results from the START2-AF registry. J Clin Med. 2024;13(7):2009. doi: 10.3390/jcm13072009.
Rieser KN, Rosenberg EI, Vogel Anderson K. Evaluation of the appropriateness of direct oral anticoagulant selection and monitoring in the outpatient setting. J Pharm Technol. 2017;33(3):108-13. doi: 10.1177/8755122517698976.
Moudallel S, Steurbaut S, Cornu P, Dupont A. Appropriateness of DOAC prescribing before and during hospital admission and analysis of determinants for inappropriate prescribing. Front Pharmacol. 2018;9:1220. doi: 10.3389/fphar.2018.01220.
Elfar S, Elzeiny SM, Ismail H, Makkeyah Y, Ibrahim M. Direct oral anticoagulants vs. warfarin in hemodialysis patients with atrial fibrillation: a systematic review and meta-analysis. Front Cardiovasc Med. 2022;9:847286. doi: 10.3389/fcvm.2022.847286.
มรกต ฤกษรัตนวารี. ความชุกและการจำแนกอาการไม่พึงประสงค์จากการใช้ยาโรงพยาบาลสอยดาว. วารสารศูนย์การศึกษาแพทยศาสตร์คลินิก โรงพยาบาลพระปกเกล้า [อินเทอร์เน็ต]. 2558 [สืบค้นเมื่อ 12 เม.ย. 2567];32(4):332-47. สืบค้นจาก: https://he02.tci-thaijo.org/index.php/ppkjournal/article/view/67729
Alberts MJ, Bernstein RA, Naccarelli GV, Garcia DA. Using dabigatran in patients with stroke: a practical guide for clinicians. Stroke. 2012;43(1):271-9. doi: 10.1161/STROKEAHA.111.622498.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Health Administration Division, Office of the Permanent Secretary, Ministry of Public Health and The Society of Hospital Pharmacist, Ministry of Public Health

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
ข้อความภายในบทความที่ตีพิมพ์ในวารสารเภสัชกรรมคลินิกทั้งหมด รวมถึงรูปภาพประกอบ ตาราง เป็นลิขสิทธิ์ของกองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข การนำเนื้อหา ข้อความหรือข้อคิดเห็น รูปภาพ ตาราง ของบทความไปจัดพิมพ์เผยแพร่ในรูปแบบต่าง ๆ เพื่อใช้ประโยชน์ในเชิงพาณิชย์ ต้องได้รับอนุญาตจากกองบรรณาธิการวารสารเภสัชกรรมคลินิกอย่างเป็นลายลักษณ์อักษร
กองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข อนุญาตให้สามารถนำไฟล์บทความไปใช้ประโยชน์และเผยแพร่ต่อได้ โดยอยู่ภายใต้เงื่อนไขสัญญาอนุญาตครีเอทีฟคอมมอน (Creative Commons License: CC) โดย ต้องแสดงที่มาจากวารสาร – ไม่ใช้เพื่อการค้า – ห้ามแก้ไขดัดแปลง, Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0)
ข้อความที่ปรากฏในบทความในวารสารเป็นความคิดเห็นส่วนตัวของผู้เขียนแต่ละท่านไม่เกี่ยวข้องกับกองบริหารการสาธารณสุข สำนักงานปลัดกระทรวงสาธารณสุข และ ชมรมเภสัชกรโรงพยาบาลกระทรวงสาธารณสุข และบุคลากรในกองฯ หรือ ชมรมฯ แต่อย่างใด ความรับผิดชอบองค์ประกอบทั้งหมดของบทความแต่ละเรื่องเป็นของผู้เขียนแต่ละท่าน หากมีความผิดพลาดใด ๆ ผู้เขียนแต่ละท่านจะรับผิดชอบบทความของตนเอง ตลอดจนความรับผิดชอบด้านเนื้อหาและการตรวจร่างบทความเป็นของผู้เขียน ไม่เกี่ยวข้องกับกองบรรณาธิการ



